SARAH: This is At the Core of Care. A podcast where people share their stories about nurses and their creative efforts to better meet the health and health-care needs of patients, families and communities.
I’m Sarah Hexem Hubbard with the Pennsylvania Action Coalition and the Executive Director of the National Nurse-Led Care Consortium.
As part of our special vaccine confidence coverage, we’re taking stock of the latest vaccine confidence trends and some of the lessons learned so far during this public health emergency.
On this episode, Annette Gadegbeku is joining us for a community-health focused conversation regarding her work to promote vaccine confidence.
Annette is a family physician and an associate professor at Drexel University in Philadelphia. In addition, she holds various leadership positions at Drexel, including being:
Our producer Stephanie Marudas spoke with Annette.
STEPHANIE: Thanks Sarah. Annette, welcome to At the Core of Care.
ANNETTE: Thank you for having me today.
STEPHANIE: So here we are recording this conversation. It's January 31st, 2023. President Biden has made inklings that the end of the COVID-19 Emergency could happen as early as May. Where are we?
ANNETTE: Yes. That is an important announcement that will come. And things have definitely evolved and changed over the years with COVID. And it's important to still be aware of the virus, its risks, and how to continue to protect ourselves, our communities, our families, our patients and those that we serve, um, even more now than ever.
STEPHANIE: Yeah. And you, from the get-go, when the pandemic hit have been very active in various initiatives. And we'd love to hear about your experience, in rolling out some vaccination and testing initiatives at Drexel, that helped serve the community. And specifically at the Dornsife Center for Neighborhood Partnerships where you helped oversee the launch of mobile clinics.
Can you share with us some of the key community health lessons learned about rolling out these types of initiatives?
ANNETTE: So, previously, I was medical supervisor at the Dornsife Center’s Community Wellness Hub. I was there for several years prior to the pandemic. And even then, I learned about how to really assess and address the needs of the community through developing programming that was important to the community and the community's health surrounding the center, and particularly Drexel. As we study and work and learn in that community, we need to partner with the community that we are neighboring and also serving and important to learn from them as well.
So, some of the lessons learned about just implementing any community initiatives, service, programming, whatever it is that one chooses to do, it's really important to hear the voice of the community and to build trust. I think if I could whittle things down, there's so many things that are involved in this work, but if I could put at the very top is hearing voices, and building trust.
And what does that look like? It can vary, definitely. But understanding that this is a partnership, in that we are here to learn from each other, work with each other and to provide service and learn in the best capacity that we can with each other to provide the best health opportunities for our communities.
Some of the ways that we did this at the Dornsife Center Community Wellness Hub, under first Dr. Loretta Jemmott, who came and did a very comprehensive assessment of the needs. That is usually one of the first steps in any kind of community engagement. We, as particularly healthcare professionals, we like to think that we know and we like to do good things. We sometimes get ahead of ourselves in thinking we know what's best for communities and others, but it's really important to pause there and to really hear the voices and assess the needs and find out what has been done. What has not been done? What has worked? What has not worked? And how the community wants to assist you in implementing the wonderful ideas that everybody has in serving and utilizing the community. Not just going in, putting something together, implementing something, particularly going in making changes and then leaving.
And that leads to just building trust. And how you do that is just having multiple conversations with key community stakeholders. Community leaders, those who are already trusted in the community, whether they’re civic engagement leaders, whether they're pastors, block captains, whether they're already community health workers in the neighborhoods. And getting that validation that we are to be trusted and we are here to truly help and partner with the community to provide a service.
We did that also by having some weekly sessions at the Dornsife where people could walk in and ask questions. We called them Ask the Doc, and at one time we did have a nurse there. So Ask the Doc, Ask the Nurse sessions where people could walk in and ask their questions and get consultation and ask about medicines, ask about their health, ask about their numbers. And then we expanded that to some physicals, especially providing physicals for people to have employment, employment physicals, and get the tuberculosis screenings with PPDs.
We also had some community health chats. They were started out in person and then of course continued as the pandemic hit and continued. We transitioned those to virtual health chats. But these were sessions that were available. And I think we started them virtually, even before the pandemic, which was truly helpful because that was already established and people didn't have to make such an adjustment to attend these sessions.
But these were sessions where we would provide information, have some experts or consults and provide a platform for discussion for anybody who would like to join, to learn more about their health, learn more about health conditions, about wellness, various topics. And then got to see, um, again, a familiar face and a consistent face.
One of the other keys to community engagement is being consistent and showing up. And so, when people got used to seeing, I think, me and others, they knew who we were and maybe hopefully felt that we were giving great information and wanted to come back week to week to hear more.
And then, we were also a face that was in person that they could come to the Wellness Hub to see and to ask questions. So I think those were important steps and foundations that we established, particularly at the Dornsife Center, to build that community, to build relationship, to build partnership, and most importantly to build that trust.
STEPHANIE: So what we're hearing here is a multi-pronged approach that combined in-person events, virtual events, consistent events to build that trust. And to go back to one thing that you said about, early on the comprehensive assessment of needs was happening, learning what didn't work in the past and what did work. And here we were in the pandemic, pretty urgent, you know, to figure out, okay, how are we going to do this right? Curious to hear what some of those things were that hadn't worked in the past and where you could tread some new ground.
ANNETTE: Yeah, I think some of those things are just reinforced in what I mentioned. What definitely did not work and does not work is coming in, kind of feeling like, particularly as a large institution and a university, we're coming into your community, we're coming into your space, we're taking over, we're doing things and leaving or not following up.
And most importantly, too, we're collecting information, right. I'm talking about needs assessments. So we're surveying, we're asking questions, we're doing these things, but then the community doesn't hear back on what we've assessed and then what are we going to do about what we assessed. So that was really important and I think key, particularly at the Dornsife Center, in going back to the community, presenting what it is that we've learned, and how we're going to help. Proposing how we're going to address and then actually addressing it. And showing that we're here. One of our slogans is, ‘we're here because we care.’ But really not saying that in just words, but doing it in action.
So, that was one thing that was made very clear from the community voices that they did not want us coming in here. Doing things, disrupting their lives, giving hope, all those things and not being sincere. Not being consistent and then not really developing relationship and partnering and that means having continued conversations, not just getting that data and getting that information, doing something with it and moving on.
They wanted to be a part of the process. They wanted to have their voices heard. They wanted to know how they could be involved. And so, the things that we've done, we've definitely tried to incorporate the community and partner with them in anything that we do and listen and act on what they've said.
STEPHANIE: So, really creating this level of transparency, maybe transparency plus agency at the community level. And sort of segueing to the launch of mobile clinics as one of the solutions, is that something that came up as, you know, needing flexibility and sort of meeting that need to meet people where they are.
ANNETTE: Exactly. In my work, I’m a huge advocate for meeting people where they are. And as I continue to do this work, I continue to see where disparities and gaps are widened because of whether it's access, whether it's trust, whether it's misinformation, whatever it is that prevents the opportunity for people to engage with the healthcare system. And people are, are just not always coming. Even as we address those barriers, to come to our centers, to come to our offices, to come to our hospitals. There's some level of either hesitancy or inability or even a lack of desire or trust to go.
So, I believe how we can start to deliver healthcare services and support and education, counseling, all those things is to go meet people where they are. And not keep waiting for people to come to us because there's still going to be a subset of people that are not going to come. And so, yes, that was one of the basis for developing these mobile outreach, particularly for testing and vaccination through our mobile team during the pandemic. Of course, another motivation was just seeing communities, particularly those black and brown, and especially black and African-American communities in our own city, having higher rates of COVID infectivity and lower rates of vaccination when vaccines became available.
And knowing the statistics of the higher morbidity and mortality of our community, really being impacted from this virus. And I think with what I mentioned about what we had developed at the Dornsife Center, luckily we had already kind of had that foundation and so we were able to expand on that and use that foundation and the platforms that we had already established to hear the voices, to hear the concerns, to hear the questions, and to have a platform that enabled us to deliver good information, trust and information. Timely information and dispel myths and misinformation during a grave time of uncertainty and fear and anxiety and mistrust and distrust.
And so, we were given the opportunity by applying for a grant through the Department of Health in the city of Philadelphia. They were calling for people to propose programs to help with the disparities and what we were seeing and the impact of COVID. And so, I wanted to bring services where they were needed. So, we assessed our communities. We found that around our neighboring community were areas of that high infectivity, low vaccination rate when vaccines became available. So we wanted to make an impact in those areas and try to eliminate the barriers for testing and eventually vaccinations. So, we set up shop. First, we set up right outside on the lawn of the Dornsife Center in the parking lot. And we just showed up, and we showed up consistently week after week to provide testing. And we saw our numbers grow over time and definitely boom and explode during the surges that we had during the pandemic.
And so, we used that philosophy of meeting people where they are, showing up, being consistent, seeing where the need was and addressing it in the best way that we could find and know how at that time.
STEPHANIE: So in partnership with the city, you were able to launch these clinics, to address access issues as you indicated. And to actually run the clinic, what did you have to do? How did you staff it? Like what were the operational logistics that you also had to manage? I'm sure that takes a lot of coordination and what did that involve?
ANNETTE: So, luckily, we had the funding from the Department of Public Health in Philadelphia. We used that funding to, you know, hire staff, a team of testers. We had a program manager to help just coordinate the activities. But what was our pride and joy, I think, of our team was actually our volunteers. We utilized student volunteers from across the university. We had medical students. We had nursing students. We had public health students. We had undergraduate pre-med students, and other graduate students that came to help and volunteer in whatever way they could. Whether it's helping with registration or flow or giving out education materials.
We also had family medicine residents cause I'm in the Department of Family Medicine, and we made this actually a part of their community medicine curriculum to go to the sites.
And it was me and another physician, Dr. Ted Corbin, who is now moved to another university, but we particularly established the site at the Dornsife Center. Although we had other mobile sites in other areas, particularly West Philadelphia and other sites. But we were key, not just because we were doctors, but actually because we were African American doctors. And I think that held a lot of weight with the community. And thus, we also targeted our volunteers. We accepted all volunteers, but most of our volunteers were of the underrepresented communities. And, interestingly enough, we found that our participants that came through our testing and vaccinations very much mirrored the demographics of our volunteers. So, whether that's coincidence, I really actually don't think so, but I think it definitely was a contributing factor.
So, yes at first, we just had very meager operations. We set up tents, tables, chairs outside. And then, eventually as weather started to become a factor, we were able to secure a space within the Dornsife Center indoors.
And we had a place to have our testing and a place where people could wait for their results. And the biggest thing was it was free. And it was free because at that time, testing was free for everybody without insurance. And we had the supplies and we had the testing materials. We partnered with the lab, with LabCorp if we needed to send out any kind of specific P C R testing, depending on the situation of each individual.
So, I mean basic operations, and not to say that this was novel. We weren't the only ones in the city. I acknowledged that doing this. But there was not a lot. And at one point we were maybe one of very few and even only at some point during the pandemic, in our area that was providing free testing. And that was key. That was important as well.
STEPHANIE: It's interesting because throughout the past few years when we've been doing COVID-19 coverage on At the Core of Care, some issues have come up about how there were limited opportunities for residents or younger training medical professionals. So this clinic, this seemed to be able to amplify in a way where you maybe wouldn't see otherwise.
ANNETTE: We did, and that was one of our goals. We had some stated goals, of course, to meet the needs of the disparity we're seeing amongst the community for COVID. But we also heard and felt the desire of our health professional students wanting to help.
And the students’ across the city, experiences were varied depending on their institution and what they were able to do, what they were allowed to do, what they wanted to do. But Drexel is a very civically engaged institution. Our students wanted to be out there and wanted to help. And there were very limited opportunities for students to do this community engagement safely. And there were a lot of concerns about exposure for our students and liability and things like that. But yes, we were not only able to provide a service for our community members, but we were also able to provide an opportunity for students to serve, to give back, and again, learn from the community and the community members that were coming through.
And they learned to, not only how to engage, but to speak to people. They had to be up to date on their information. We were able to teach them as the guidelines and recommendations changed throughout the pandemic. You know, they were very engaged. Were asking questions and learning from us and learning about what people were coming with when they came in terms of their fears, their questions, their myths, and learned how to address those with the community members as well. So it was a great experience, I think for everyone.
STEPHANIE: And we could talk more broadly now about vaccine confidence, but to sort of make the connection here, a point that you raised about a lot of the volunteers mirroring the population coming through the clinic. And that's another theme certainly we've talked about on this podcast over the past two years about trusted messengers. And being able to relate to somebody who might be like you and having that connection. And I wonder what you and your colleagues learned in terms of vaccine confidence, through the clinics and other ways too?
ANNETTE: We definitely saw the vaccine confidence increase over time. With lots of conversation, either through our chats or conversation at our site. We had many people coming back frequently or repeatedly for testing. So we had a lot of repeat participants, whether it was because they needed a weekly test for work or they were repeatedly concerned about exposure or whatever. And so we definitely used, as vaccines became available and we partnered with Sunray Pharmacy to provide the vaccines and kind of mirror that to have a parallel, side by side, operation with our testing and our vaccinations. So as people were coming to be tested, we would educate about vaccination. Particularly, seizing the opportunity if they were negative for their COVID test and offer, would you like to get vaccinated today? We can do that for you today. And you know, that started out very small, meager. And over time, that definitely increased. And again, we saw a definite mirror, as the surges came. We saw a surge in vaccination uptake, right behind it. And that was cool to see and to learn from and to learn you don't give up on it. Again, be consistent, persistent, not pushy, not aggressive by any means.
And it wasn't about convincing people to get the vaccination. It was all a part of education and providing good information. Being a useful resource where people are getting information and using varied resources and some not, you know, evidence-based or some not very reliable. But being a consistent source of good information where we could just provide and have the conversations that people needed to have to get their own ideas and to use what information we give to make their choice.
We just wanted them to make the best-informed decision for themselves. And we did. We saw people come. Especially those that came multiple times, you know, the first time they were maybe like, absolutely not. But then we saw it change to, mm, let me think about it. And then we definitely had people that after a few times came and decided, for whatever reason, it could have been us, you know, we might be at any time planting a seed, watering a seed, helping to prune a plant in that area. Or they may have had an experience that kind of changed their mind about what to do. But the important thing is that we were there to bounce off questions, ideas, concerns, myths, and we were there to provide it when they were ready. And we definitely saw that.
So that was definitely cool to experience. And again, people sought us out, particularly those who are underrepresented that were there to ask ‘what did we think,’ ‘what did we feel,’ ‘what did we recommend?’ And again, it wasn't about convincing, but just giving informed information for them to make the best choice for themselves.
STEPHANIE: Yeah, I mean, it comes to one of your original points of the conversation about trust and you know, if there's somebody who can come and talk without judgment and just getting the facts.
ANNETTE: It was definitely good to see the shift and the change over time. And to be able to be available, to calm people's anxieties and fears and to see a transformation sometimes. And also just to have a pleasant conversation, regardless of what the outcome is. And again, just be available, for whatever is needed in that moment for people.
STEPHANIE: Yes. And you know, on that point, people who came to the clinic might end up having future healthcare experiences with you and your colleagues for their general health. Like you said, this is not a one-off, this is an ongoing relationship.
ANNETTE: And it is definitely something that we are trying to expand upon. What was really cool is one of our student volunteers from the very beginning, she created a website, and collated important informational resources for various needs. What we saw, of course, during the pandemic was a lot of the other disparities kind of just be magnified. Whether it's financial challenges, housing challenges, nutrition challenges, all these things, just magnified for our community. And so, some of our materials were geared towards helping, addressing, directing counseling for other needs. Whether they were health needs or social service needs. And so we were able to put all of that with a pamphlet and we used a QR code to direct people to those resources that they needed. And as we are continuing the operation in a slightly different way, but we're continuing our testing and vaccination at the Dornsife, we are definitely looking for ways to expand those services to address other healthcare needs, health conditions, screenings, and providing education and counseling in other areas. One of which, we got another funding opportunity to provide M-pox vaccination, along with our operation at the Dornsife. So we are actually officially starting that this week.
And then, again, we married those throughout the pandemic as well when we would do pop-up sites. We would have health screenings, blood pressure, glucose screenings, and then also our testing or vaccinations. So we did those for various pop-up events throughout the pandemic, particularly in the more seasonal months where we were able to be outside for those community health events. You're right, it's not a one and done, it's not a one-off, it's not a one condition or area type focus. We are definitely using the opportunity as we engage with the community to educate, counsel and provide other services for other things that they may need.
STEPHANIE: Keeping that in mind, Annette, as we talked about at the top of the show, you know, the end of the COVID-19 health emergency is coming. So what do things look like now, you know, how do healthcare professionals talk about COVID-19 and vaccines as part of routine healthcare? And certainly there has been a change in people's decision to get boosted further at this point.
ANNETTE: That conversation has definitely evolved over time. What that conversation looks like, sounds like is quite different and variable. Particularly now, at this current time, we've seen people's decisions get a little bit polarized by now. There's not a lot of conversation centered around so much information or trying to assess and address people's confidence or hesitancy. Because many people have made up their minds whether they're getting vaccinated or not. And I think we're at a time where I think people have heard as much as they feel that they need to make that decision. There are still a few people that can be in between. So, I think having the conversation is still important. Bringing it up is still important and I'm going to say how and why in in a minute. But just addressing where people are. I think people are a bit in a state where they kind of know what they want to do. They're pretty confident in what their beliefs and their comfort level is on the vaccine.
However, with every change, with every shift or transition, there brings more opportunity to have those discussions again. Like, this season, for example, we know that COVID increases during the fall and winter months. And so, we have other vaccines like the flu that we tend to offer and have conversations about.
And people are getting sicker during those months. And those are opportunities to have the conversation or when the new booster came out, that was an opportunity to have the conversation. But, I think shifting even away from situational conversations and making them more routine I believe is the way to go. That way that we're moving and the way that we should go. We know now that COVID is here and it's not going away. What it looks like and feels like for people may vary and change, but it's here. There's still risks involved with contracting the virus.
And, there's definitely risks for Black and brown communities. So, the conversations still need to occur, but it shouldn't be taboo, it shouldn't be situational. I think at this point it should be routine and that's what we're seeing. Some of the guidelines and the recommendations recently are coming out. It's going to be a part of the vaccine schedule. So we have all these other vaccines that we routinely provide and offer in a well visit or an office visit to providers. And so, making this now a part of your routine health conversation in an office visit. And you know, maybe we will get away from any stigma or stigmatized conversation around the vaccine.
STEPHANIE: How about access? You know, the government has covered a lot of the testing and vaccination. If this health emergency comes to an end, maybe things aren't defined yet, in terms of how, people who may not be able to afford a vaccination or testing, you know, how will they be able to access those health services?
ANNETTE: It's definitely something that we need to keep an eye on as policies change and coverage changes. We definitely saw that even while we were still providing our mobile testing, whether now the grant for the testing agencies to cover the vaccine had ended and so we had to go use people's insurance. And what about those that didn't have insurance? Luckily, there was another lab we could use to process tests. So, I think access to similar operations means mobile clinics I think are still going to be important going forward as that changes. We do have some initiatives coming through the city. I think some people are still being sent COVID home tests, and some offices and some of the health department and community health centers are able to provide testing for patients regardless of insurance. So, making sure we have that available for our patients is going to be important in our community.
I was a little sad and disappointed that the funding stopped in December. I think it's still going to be a need. I think regarding access or whatever it may be, because we're in close proximity with community members, being able to just walk up and come get tested or insurance. Granted our numbers did decrease significantly last year, which is a great thing and I think that's hopefully due to greater access or decreased need for it. Like I said, I think there's more access to home testing, home kits and things like that, so I think that contributes. But just wanting to be available again for those that need it and don't have that access. But just having it available. And I think that's why I'm happy that we're able to transition it to the Wellness Hub, who will continue those services regardless, and they'll have that available to utilize for the community. So, it's something that we need to keep an eye on and make sure that we're not leaving anyone out that needs those services.
STEPHANIE: As we take what you just said into consideration and all the various topics we touched on throughout the show, what might you want to leave listeners with in terms of any final thoughts, especially as we're here at this point, early 2023, going forward.
ANNETTE: I think it's a time we are feeling a bit relieved and less urgency about COVID and the virus. However, it's not the time to take our foot off the gas for continuing to educate and counsel and provide opportunities for people to stay safe, and particularly those populations that are marginalized and vulnerable. We need to continue to provide access, information, education and whatever services that we can provide for people and then also to continue the conversation.
I think it's a conversation that's worth having and worth bringing it to be a part of our routine healthcare and health maintenance. Our goal every year is to help all achieve their best health. That's what health equity is, and so the best, best health that they can achieve. And this is a part of it. This is a piece of it, but it's a part of assisting people to get to that health equity status where they're achieving their most, best health and wellness. So, always looking for the opportunities to not only engage, but to partner. And to provide and to learn, with our communities to achieve our best health.
STEPHANIE: Thank you, Annette, for sharing all your perspectives with us today on At the Core of Care. We really appreciate you making time to have this conversation with us.
ANNETTE: Thank you. Thank you for having me.
CREDITS
SARAH: Our special Vaccine Confidence series was funded in part by a cooperative agreement with the Centers for Disease Control and Prevention or CDC. The CDC is an agency within the Department of Health and Human Services also known as HHS. The contents of this resource do not necessarily represent the policy of CDC or HHS, and should not be considered an endorsement by the Federal Government.
Stay tuned for more episodes coming up in our vaccine confidence series. We’ll continue talking to healthcare professionals and frontline workers who are addressing issues that were exacerbated by the pandemic and promoting vaccine confidence.
You can find our most current and past episodes of At the Core of Care wherever you get your podcasts or at paactioncoalition.org.
And for more information about related upcoming webinars, COVID-19 resources, and upcoming trainings for nurses to obtain continuing education credits, log on to nurseledcare.org.
You can also stay up to date with us on social media by following @NurseLedCare.
At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder.
I’m Sarah Hexem Hubbard of the Pennsylvania Action Coalition.
Thanks for joining us.
SARAH: This is At the Core of Care, a podcast where people share their stories about nurses and their creative efforts to better meet the health and health-care needs of patients, families and communities.
I’m Sarah Hexem Hubbard with the Pennsylvania Action Coalition and the Executive Director of the National Nurse-Led Care Consortium.
As we enter the third year of the COVID-19 pandemic, we’re going to spend the next four episodes taking stock of the latest vaccine confidence trends and some of the lessons learned so far during this public health emergency.
Joining us for this conversation is Melody Butler.
Melody is a member of the National Vaccine Advisory Committee as well as a member of NNCC’s Vaccine Confidence Advisory Committee. More than a decade ago, she founded and still runs Nurses Who Vaccinate. She’s also a registered nurse and infection preventionist on Long Island in New York.
Melody, welcome back to At the Core of Care.
MELODY: Thank you. I'm very happy to be here.
SARAH: So, Melody we last spoke about two years ago in 2021 when we kicked off our COVID-19 vaccine confidence coverage. Clearly, a lot has happened since then. There's now even a word we didn't have two years ago: tripledemic. From your perspective, how would you describe where we are now?
MELODY: Well, we've learned a lot since 2021, and we have a lot more tools in our toolbox to protect ourselves against all of these respiratory diseases that we're concerned about. When you talk about the tripledemic. So flu, COVID, RSV, we know how to bring the rates of infection down and we know what we need to do in order to protect the most vulnerable in our communities.
Unfortunately, not much has changed in regards to vaccination rates. Last we spoke, the vaccination rates for United States at the end of 2021, we were about 73% for people having had received at least one dose of the COVID vaccine. And here we are in 2023 and we're at a whopping 81% of people having at least one vaccine dose.
So, I'm very disappointed to see where we are right now. The fact that we have not hit at least a good 90, 95%, like we have with other vaccines, unfortunately. So that goes to show you that there is so much work that needs to be done.
We have hit a couple of walls. The public's confidence in the vaccines and in boosters have taken a hit due to variants and surges.
And the data that I really want to highlight throughout this talk, especially when we talk about the COVID vaccine, is how, while it may not protect you from getting sick, you may still catch COVID, despite being vaccinated but it's going to do an amazing job keeping you out of the hospital. It's going to keep you from developing severe illness, complications that could follow had you not been vaccinated.
SARAH: Hard to pinpoint exactly. But it seems like people are sicker than before with the flu going around, COVID, the common cold. Do you agree with that?
MELODY: I do. In fact, we're in a very rough flu season. To date, today is January 24th. For this flu season, we've had a total of 85 pediatric deaths. That's awful. Last year, for the flu season of 2021 to 2022, there were 45. We haven't even hit February yet, which is normally our peak for flu season, and we have more than doubled the pediatric death rate from last year. I really do fear because usually, what we saw before when we had a bunch of Flu A. And what tends to follow Flu A is Flu B and that's going to be rearing its very ugly head very soon.
Now the thing with flu is there's no in between for flu. Either you have the flu or you don't. There's no, Hmm, I might have the flu. If you have the flu, you're knocked out, you're sick at home. However, you're contagious for about two days before you can show symptoms sometimes. So think of all the people you come in contact with in two days.
And I do worry though, because now thankfully the flu cases are coming down, but Flu B is known to piggyback on top of Flu A. So, a really important message that, uh, we need to get out there to the public is that even if you have had flu earlier this flu season, you are, um, even more at risk for complications should you catch an additional flu strain later in this season.
SARAH: And what have you been hearing and seeing in response to the new COVID-19 bivalent booster? How's it being received? What are the risk calculation conversations sounding like?
MELODY: The rollout of the COVID booster, the bivalent booster, has been very tricky and there's still lots of confusion surrounding it. And unfortunately, a lot of people still don't know that they are a candidate for it when they very much are. There's really four reasons. One is they don't realize that they should be getting it. Maybe they got a vaccinated earlier this year with one of the earlier boosters, and they don't realize that they're a candidate for this current one. Number two is they're too busy. Unfortunately, access of the booster is not as easy as it had been earlier in the pandemic. Some locations only have the booster being given out certain times and certain days of the week. I know that even doctor's offices don't always carry the booster. You go to the doctor's office for a physical and then they say go to the pharmacy to go get your booster. And people aren't making that second trip; which then leads us to number three. People are forgetting that they need the booster. Then, number four, people are worrying about side effects.
SARAH: And also side effects that can make it difficult to work. I mean, combining that, with being busy. If you know that you're someone who's going to be sick for a day or two after you get your booster, sometimes that's extra hard to schedule in.
MELODY: Of course. And we know we don't have that leeway that we once had with the original COVID vaccines, where there was even days allotted by some businesses that if you got the COVID vaccine, if you developed a fever the next day, you were not penalized. And it was okay. It was recommended that you actually stay home and recover from getting the vaccine because they realized how important it was to get vaccinated. And it kind of seems that we've gotten away from that. It's an all hands on deck and we learned in the early days of the pandemic how to work all hands on deck.
SARAH: I think you touched on several things that were really important there, but kind of what stood out to me was that frustration. And, and it touches on a little bit of what we talked about in some of the past seasons too, about the burnout, the burn down, the fatigue. Like how could this have gone? And what do you say to your colleagues who are struggling, who are frustrated, you know, who are feeling alone?
MELODY: We all need pep talks. No matter where you are, no matter how you're working in this field, whether you're doing frontline nursing care, quality work, data reporting, public health, public education. Seeing the statistics, knowing your loved ones are getting sick, seeing family members refuse to get vaccinated then develop complications. All around, it can be frustrating and we always need to help support each other. So when we keep that in mind, we need to really make sure that we're building upon all the resources that we need to have laying out there for us, because we never know when we're going to need to step back and then tag in our partner to kind of go in there for us to kind of take over the education or take over the patient care. It’s something we need to make sure that we do a better job, relying on one another and using all the different skills that we have. I really want to say going forward, for the next winter, like let's say we know that this is going to happen again, we need to have more resources for nurses to have downtime, for doctors to have more flexibility of sick time, right?
We had even healthcare workers getting very sick during this last surge, and they were doing everything they can to protect themselves. Unfortunately, sometimes you're still exposed at home or in the community and making sure people know that they don't and shouldn't go to work sick. Making sure that we're really reinforcing and encouraging and highly encouraging self-care. So if we take away anything from this most recent winter, it's the continued need of taking care of each other, taking care of ourselves, because we're in this for the long run.
This is our new normal. And as much as I hate that expression this is it. This is what we have to really kind of focus on and come up with a good game plan in dealing with.
SARAH: And clearly, you've talked about the impact of illness on kids that we're seeing. So, looking at vaccination, I think specifically COVID-19 vaccination, how's that looking for kids? Especially under the age of five.
MELODY: So as of January 2023, the American Academy of Pediatrics continues to recommend the COVID-19 vaccine for all children and adolescents six months of age and older. As long as they don't have any other contraindication to vaccines. With that being said, right now, we have about 1.9 million children, six months to four years, who have received at least one dose. 1.9 sounds like a lot. Unfortunately, that represents only 11% of that age population.
So that means there are 15.2 million children between six months and four years to receive their first COVID-19 vaccine. And what's interesting is that vaccination rates really do vary from state to state. You have some states that are at 2% and you have some states that are at 40%. So there is a lot of work to be done. And when we talk about COVID-19 vaccine for the children under five, it's really important to stress to the parents when we're educating them, making the recommendations, is how safe the vaccine is, how we continue to monitor the vaccine for any type of adverse reactions or safety issues and whatnot.
SARAH: So thinking again about kind of where we are now and where we've been, access has been a barrier throughout the COVID-19 vaccine rollout. So, to what extent is vaccine access still an issue? Really, access to both vaccines and testing? And how do you see that changing as the public health emergency declarations are starting to expire?
MELODY: So, I've come to learn that, you know, I live in New York where everything's pretty much centralized. We have pretty good access here, and it's very easy to forget how rural some parts of the country can be. Well, a lot of the parts of the country are. And in talking to colleagues around the country, I know that it can be very difficult right now as we stand to get boosters, to make appointments, to have that availability to drive an hour or so to a vaccination site to get vaccinated. So, when we talk about the emergency declaration ending, I'm really concerned. There's going to be major changes that are going to occur. The COVID-19 federal emergency declaration provided free testing. It provided free vaccines and even free treatments such as some of the antibody treatments that people were receiving. What's important to know is not all of these items will go away, but a lot of them will no longer be free. So people, if you don't have insurance, they'll no longer be a pathway through Medicaid for free COVID testing, vaccines or treatments. And then for Medicare beneficiaries, there is going to be a cost sharing requirement. Hospitals are going to be affected by this. Hospitals will no longer receive the 20% payment increase for discharges of patients diagnosed with. when this expires. And we know that when you have a COVID-19 patient, it's complicated. So, to lose that funding that can help provide for additional nursing care, that's very troublesome. It's something we should be worried about. And, you know, I mean that's just a small snippet of the concerns that I have when this does expire.
SARAH: So, as we're forecasting out, you know, what are the things to be paying attention to, what might we expect to see in terms of vaccine confidence trends? You know, the next six months, the next year, what do you see coming?
MELODY: I foresee us in the healthcare community having to continue this uphill battle. We are continuing to push against misinformation. We have to push against this adversity to mandates. And also we have to push against hopelessness that we see in our patients. People are very disappointed that the COVID vaccine does not prevent illness. We have to stress how amazing it is that the vaccine keeps you out of the hospital just like the flu shot. The vaccine prevents severe complications and it prevents death. It does a great job at keeping you alive, and that's such an important point that we need to stress to the public, to our patients, to our communities. But we need to do a better job at that. And we need to continue to push back even harder against misinformation. The misinformation and the anti-vaccine movement organizations, they're only getting stronger. Social media has its ebbs and flows in regards to how it regulates and how it decides what's acceptable and what's not acceptable. And unfortunately, right now we are dealing with really, really serious conspiracy theories. And it's very damaging to the public's confidence. So, we need to have a more collaborative effort in pushing back against these very negative narratives and sharing stories of how safe it is and how important it's to be vaccinated. And how being vaccinated is one of many of the tools we have to protect ourselves. Hands, hygiene, washing your hands, wearing a mask. Being aware of your surroundings in a crowded area. I, myself, when I go to shows and if I'm like, you know, attending a, a musical or a play, or even a concert, like my kids' concerts, sometimes those auditoriums can be very packed and you’re right on top of each other. I put a mask on because I know I'm going to be in this one spot for a good two and a half hours.
I hear the person behind me coughing and sneezing, you know what? I don't want it. I don't care what they have. It could even be a mild cold. I don't have time to get sick. I'm going to utilize all these tips and tricks that I have, you know, using Purell. I'll carry Purell with me and wash my hands.
So, we need to continue to really educate the public. We need to really work together and to continue to encourage one another to be vocal advocates whenever we can.
And if you yourself don't know the answers, at least know where to direct people to go. At NNCC, there are many resources that people can utilize in regards to updating themself, webinars, and other educational pieces they can use to stay up to date.
The CDC has a great reference. They're called the COCA Calls where they put out on a monthly basis keeping everyone up to date on the effectiveness of vaccines. And the latest outbreaks and important information the healthcare providers need to know. Vaccinate Your Family is another great resource that we direct people to go to. They have a lot of information that's easy for the common lay person to read. You don't have to be in the medical field to understand the information they put out there. And if you're looking for like-minded people who are vaccine advocates, who appreciate the science, maybe don't have a huge scientific background, but you want to do your part. There's an organization called Voices for Vaccines that I'm also a part of that we work really hard to just encourage the regular person to be a science advocate.
SARAH: Can you tell us a little bit about Nurses Who Vaccinate? What's going on with that right now?
MELODY: Thank you for asking about Nurses Who Vaccinate. We are sharing some very important information on our social media pages, making sure that our members and our followers are staying up-to-date on what they need to know about COVID and flu, RSV, Monkeypox. We continue to be a reference point for nurses and healthcare workers to collaborate to come up with ideas and a game plan in regards to education and advocacy, whether it's in their own workplaces, in the community, in the nursing field. We're working with organizations to host some events that are up and coming, so stay tuned with that. We're looking forward to hosting HPV vaccine awareness events. We're going to be looking to partner with one of our partners Shot at Life for an upcoming summit, where that’s going to be involving our members going out in the real world, doing face-to-face advocacy with some of our legislators and educating, them on what they need to know about vaccines and making sure they're up to speed on the up updates and evidence-based information. And we'll be working with our members to continue to provide that support that's very much needed, especially those who are vocal vaccine advocates. Sometimes it could be a very lonely world out there for those who are passionate about vaccines. And it's important that they know that they're not alone. And we are here as a resource, as a safe place for them to come up with great ideas that continue that momentum and get the information out there to the public and to renew their sense of service.
SARAH: So, before we come to an end, any final thoughts you want leave with our listeners?
MELODY: What I would like everyone to walk away with are three points. One, it is not too late to get vaccinated and it's not too late to convince your loved ones and family members to get vaccinated. Persistence is key and continue to be their source of information to be that place they can go to ask questions in a safe venue. Two, don't give up. Sometimes it can be very frustrating. That was our common theme of the night. But don't let the frustration keep you from doing good work. Continue to fight the good fight. We need to protect ourselves, our colleagues, our patients, and our community from these preventable diseases. And that's what they are. Number three, they're preventable and that we can only prevent them if we use all the tools in our toolbox. So, remember, it's not just about vaccines. It's about wearing a mask. It's about staying home when you're sick. It's about washing your hands. The simplest of simple things. I want to make sure that people understand all these things do add up and they can play a huge part. Making sure good ventilation systems. Oh, we could talk an hour about that. Even more than that, right? I wish we had the time. But working together to put all the pieces of the puzzle together, and hopefully maybe next winter, we won't see the crazy surges that we saw, and we won't have 80 kids dying from the flu.
SARAH: Thank you so much for everything that you're doing to keep this movement strong and the contributions that you're making personally and and professionally. And of course, thank you for making time to join us on At the Core of Care.
MELODY: My pleasure. I hope to see everyone out there. Stay safe and stay healthy.
CREDITS
SARAH: Our special Vaccine Confidence series was funded in part by a cooperative agreement with the Centers for Disease Control and Prevention or CDC.
The CDC is an agency within the Department of Health and Human Services also known as HHS. The contents of this resource do not necessarily represent the policy of CDC or HHS, and should not be considered an endorsement by the Federal Government.
You can find our most current and past episodes of At the Core of Care, wherever you get your podcasts or at paactioncoalition.org.
And for more information about related upcoming webinars, COVID-19 resources and upcoming trainings for nurses to obtain continuing education credits, log on to nurseledcare.org.
At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder.
I’m Sarah Hexem Hubbard of the Pennsylvania Action Coalition.
Thanks for joining us.
.png)

To celebrate Black History Month, we are honoring Black healthcare leaders who have contributed to the advancement of our health and healthcare systems. Their contributions continue to have a long-standing impact on us all. To celebrate their legacy, we will be spotlighting Black nurses, advocates, and other trailblazers and their achievements.
Learn more about the Historical Black Healthcare Leaders we are highlighting this month.
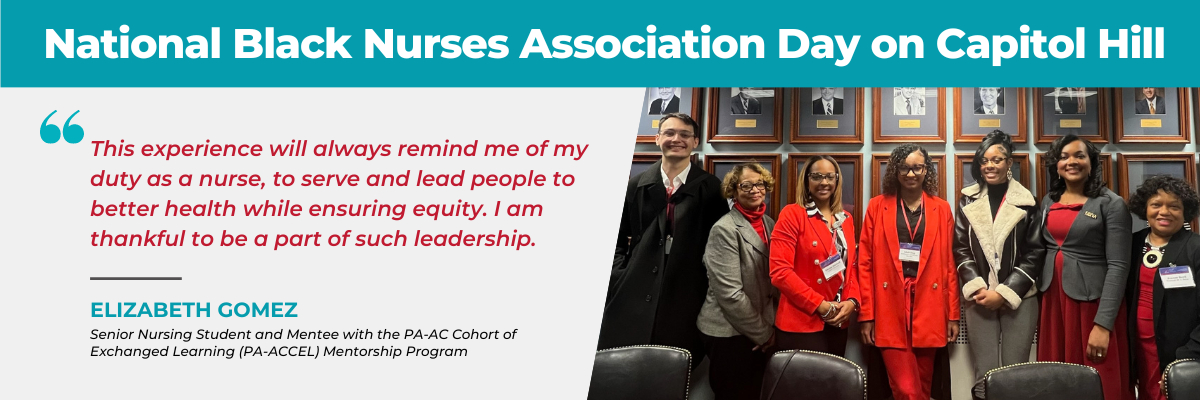
As we honor past nursing leaders, we also celebrate the future of nursing. On February 2, 2023, the Pennsylvania Action Coalition had the pleasure of attending the 35th Annual National Black Nurses (NBNA) Day on Capitol Hill. This forum is dedicated to congressional health issues and policy. Student mentees from the PA-ACCEL Mentorship Program, a partnership with Lincoln University, learned about seven key legislative priorities advancing health equity. These legislative topics included:
Mentees in the PA-ACCEL Mentorship Program share highlights about their experience at NBNA Day.
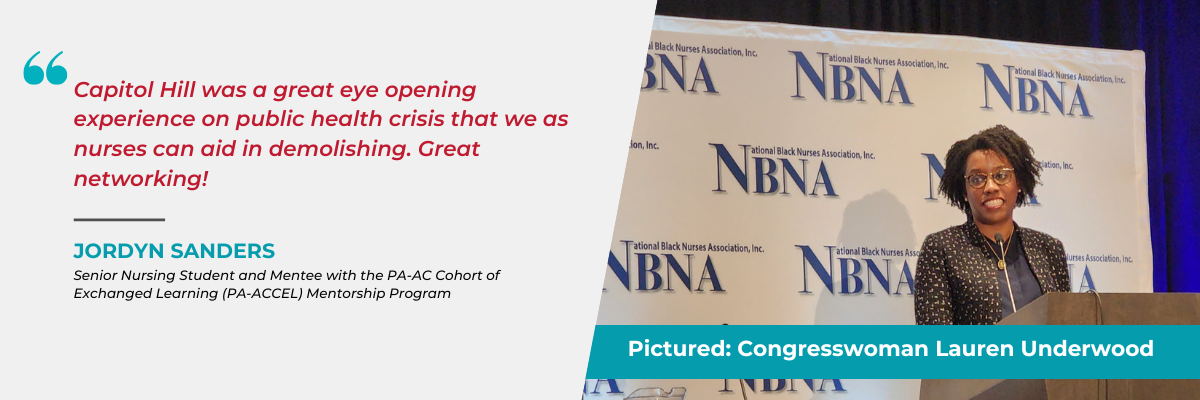
Pictured below is Congresswoman Lauren Underwood who currently serves as a member of the U.S. House of Representatives. Underwood represents the 14th Congressional District of Illinois, officially taking office on January 3, 2019. Congresswoman Underwood is a trailblazer, being the first female, the first person of color, and the first millennial to represent her community in Congress. Learn more about her accomplishments and work.

The Geisinger School of Nursing, in collaboration with the Pennsylvania Nursing Workforce Center (PA-NWC) and the National Nurse-Led Care Consortium (NNCC), is addressing nursing faculty and instructor shortages by participating as one of ten Nurse Education, Practice, Quality, and Retention Clinical Faculty and Preceptor Academies (NEPQR-CFPAs).
The collaborative is executing the program with funds awarded by the U.S. Health Resources and Services Administration (HRSA), CFDA#93.359 and is focusing on HRSA Region 3 (including Delaware, Maryland, Pennsylvania, Virginia, West Virginia, and Washington, D.C.).
The purpose of the NEPQR-CFPA is to close the clinical faculty gap by leveraging new and/or existing nurse education and forward-facing staff nurses to participate as skilled clinical instructors and/or preceptors through the development of a comprehensive, self-guided training program.
The CFPA 101 facilitates the growth and development of bedside nursing staff, nursing schools’ educators, clinical faculty, and preceptors, which in turn will improve the severe nursing shortage through stronger clinical educational opportunities that has worsened since the pandemic. The CFPA 101 aims to empower and encourage nurses to work as preceptors and clinical faculty to undergraduate PN and RN nursing students during clinical rotations and will be widely available for use by healthcare systems and academic institutions in October 2024. The CFPA 101 was created by Geisinger, PA-NWC, and NNCC.
To develop this curriculum, the PA-NWC assembled an Advisory Board reflective of diverse practice areas, academic pathways, geographic locations, and populations served across HRSA Region 3. The Advisory Board oversaw curriculum development and determined metrics of review. The PA-NWC and Advisory Board stakeholders ensured that the course content is engaging, thoughtfully articulated, and caters to a wide audience. Currently, employees across the Geisinger health system are piloting and evaluating the curriculum. The PA-NWC and CFPA Advisory Committees will use lessons learned to prepare the program for implementation across the HRSA Region 3 beginning in the Fall of 2024.
Meet the CFPA Members
We are pleased to announce that CFPA 101 is now available to healthcare systems and individual nurses in HRSA Region 3.
Eligible CFPA 101 participants include undergraduate nursing student preceptors or clinical faculty with at least an LPN or RN license in good standing. The CFPA 101 training addresses professional development needs of clinical faculty and preceptors working in a variety of settings. However, this initial version of the CFPA 101 curriculum includes teaching scenarios and activities particular to the ambulatory, in-patient setting.
The CFPA 101 course curriculum is divided into 6 modules. Some content is specific to a particular module, while other content areas carry across modules. The modules are as follows:
Each module contains clear learning objectives, interactive learning activities, periodic learner knowledge checks, and links to vetted resources. Enrolled CFPA 101 learners must complete each module in order, pass knowledge checks, and submit a series response capstone to be reviewed by Geisinger's expert reviewers. The CFPA 101 course is hosted on Geisinger's online learning management system and open to enrolled users from approved pilot testing organizations.
Nurses who enroll in and complete the CFPA modules will be awarded a certificate of completion and can receive continuing education units (CEUs) that can be used to fulfill educational requirements for re-licensure and/or nursing certifications, for a small fee. In addition to the CEUs, nurses who participate in the CFPA 101 course may be eligible for a financial incentive based on level of participation. Grant funding for financial incentive payments is not guaranteed and will be determined on a case-by-case basis with identified pilot sites.
To access CFPA 101, please go to Geisinger’s website.
If you have CFPA specific questions or need assistance accessing CFPA 101, please email .
The Clinical Faculty and Preceptor Advisory Board is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $4 million dollars with no percentage financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government.
For more information about the CFPA 101, download the flyer here.
SARAH: This is At the Core of Care, a podcast where people share their stories about nurses and their creative efforts to better meet the health and healthcare needs of patients, families and communities.
I'm Sarah Hexem Hubbard with the Pennsylvania Action Coalition and the Executive Director of the National Nurse-Led Care Consortium.
As part of our special training coverage, this episode features a conversation about Centering Trauma Literacy in the Health Center Medical Home. We’ll hear how providers and health systems can cultivate trauma-aware practices as part of their delivery of care.
My colleague Jillian Bird, Director of Training and Technical Assistance at the National Nurse-Led Care Consortium, will lead the conversation. Through a wide variety of ongoing programming, Jillian and her team help support providers working at community health centers across the country.
MUSIC UP
JILLIAN: Thanks Sarah.
Our guests for this conversation are Kathleen Metzker and Sara Reid, and they’re joining us by Zoom.
Kathleen works in Philadelphia as the Director of Integrative Health and Mind Body Services at the Stephen and Sandra Sheller 11th Street Family Health Services of Drexel University. In this multidisciplinary health care setting, more than 6,000 patients access a range of services, including: primary care, behavioral health, dental services, and health and wellness programs.
And Sara is based in Boston where she is a health educator, support group facilitator and consumer board member for the Boston Healthcare For the Homeless. Sara is a public speaker and delivers trainings on transgender priorities, including teaching medical and behavioral health providers how to provide gender-affirming healthcare.
Welcome Kathleen and Sara to At the Core of Care.
KATHLEEN: Thanks for having us here Jillian.
SARAH: Thank you.
JILLIAN: At the beginning of each episode, we always like to ask our guests why they do the work they do. Kathleen, can you start us off?
KATHLEEN: Well that's a very good question, why I do the work that I do? I think it's natural for me to want to do work that is in the service of others. There are so many people that show up for their job to get a job done, to get home, to have the rest of their lives. But remembering that we are in constant relationship with one another is a core principle in my own life. So I’ve really had the opportunity for that to show up in my personal life every day. And it reminds me that I'm alive. And that is why I do the work that I do.
JILLIAN: And Sara, what about you?
SARAH: Actually a couple of reasons. As a mother of two, grandmother of four, you know, thinking about making the world a better place and, be better than I found it is kind of like core to who I am. And also, I've spent the last 30 years in one form of counseling or another, and you know, around the issue of trauma, the medical system itself has been very traumatic, because of kind of the era that I came out in. I'm a trans woman myself, and it was just all barriers, all stigma. We were almost universally discriminated against. And, you know, I would like to be the young 18-year-old starting out with a good prognosis a good outcome for the medical interventions and, and look forward to a whole life of you know, just being myself. But it wasn't possible for me. And I guess, one of the ways I make use or reconcile the lost time of, you know, big chunk of my life is to make sure that it never happens to anyone else again.
I struggled to get to where I am. I went through six years of reparative therapy, or they call it conversion therapy, to try and kill it off. And then having come to the end of that, I went in looking for gender affirming care, and I just couldn't find it anywhere, you know, I ended up getting referred around like a hot potato. And then interacting with the community that I directly work with, I found that, you know, my story is kind of pretty average. And the stories that have been told to me, you know, I kind of wanted to do something about it. But at the time, you know, I was having the conversations I didn't have any direct way to make the medical interaction with my community better, but I've kept it in my heart and opportunities have risen, I've taken an opportunity to kind of speak to those issues and keep the people that were kind enough to share their stories with me in mind as I went forward to do some teaching, and help people understand better.
JILLIAN: Thank you very much for sharing those perspectives with us and before we dive into our discussion, let's first hear about the communities you're currently serving and what key needs you've been concentrating on addressing?
SARAH: So my entry point into working mainly with my nurses, you know, I love working with my nurses, they've been, you know, a godsend to me, and they're just some of the finest people I know. But the sort of my entry position was seeking out help. And the most welcoming, friendly place to trans care was Boston Healthcare for the Homeless, believe it or not. Absolutely no discrimination or stigma, they've been wonderful. And with that, my interaction with patients has gone two ways. One is I'm interacting with our general patient population, as well as I sit on the board of directors. So I'm, I'm like on both levels, I'm with the executives monthly and then interacting with patients and peers. And then my, you know, where my heart lives is where healthcare touches the needs of gender affirming care for trans identified people. And I've had quite a lot of experience with that over the last decade. Things are changing in some ways, but we've still got a long ways to go.
JILLIAN: And Kathleen, what are the needs you feel like are being addressed in the communities that you're serving currently?
KATHLEEN: Thinking about it through the lens of the health home, we're a federally qualified health care center. So we're operating under the assumption and the knowledge that the greater majority of our patients live below the poverty line, low-income, socio economic status. Our demographics of approximately 6000 patients, where about 75% individuals identify as Black and African American, and the rest of the breakdown, pretty much divides between white, Latino and other. But the thing we know about individuals and communities like ours, that are really up against more social determinants of health. And there's an increase in adverse childhood events, which, as we know, then impacts health outcomes of mind and body later on in life. So thinking about this through a trauma-informed care lens, operating under universal precaution. And keeping that in mind as we're interacting with our community and patients. Also the Health Center is set right in the middle of four public housing communities. We've been there over 20 years. So especially as we emerge from the pandemic, I keep reminding my team or reminding each other we almost need to act as if we just got here, right, because we're a university affiliated medical home. So there's the history of mistrust, needing to build trust and relationships. And even in the 12 years that I've been there, generations have changed. So what used to be the children of clients are now the parents of the children, and caretakers of their elders. There's, of course, the impact of the pandemic, and the increase in community violence in Philadelphia. So all of these things are impacting the well-being of the individuals in the communities that we’re intended to serve. So really keeping all of these things in mind and understanding the complexity of those needs, is really where we're landing right now.
JILLIAN: Thank you. And I always think of where you are and the organization that you're working with as being a leader in this space, for so many reasons. And hopefully, we'll be able to touch on some of those in this discussion. But kind of following in that leadership, we've seen of continual shift and healthcare spaces to try to be more trauma informed and trauma literate, and have a more holistic understanding of what being trauma aware is. So I'm curious, Kathleen, as you think about your own organization, and also this general evolution, are there some real examples at your health center where you work that you might be able to share that sort of really highlight or encapsulate these concepts and then how they look in practice?
KATHLEEN: Yes, and I appreciate the use of the word holistic. And at the same time, I think that feels from a healthcare or scientific lens, sometimes it feels a little soft. So if we could even recontextualize it in thinking of trauma informed care as a systems approach rather than addressing technical needs.
We're also talking about humans interacting with humans, which becomes complex, and cultural perspectives. And when we think of the patient provider relationship, even through a trauma informed care lens, the ideal would be recognizing that potentially trauma has impacted this individual, their behavior, their health outcomes.
Then we have the provider patient relationship that has inherent power dynamics. So when we're considering communities that would otherwise be considered marginalized or disenfranchised. These kinds of buzzwords of people being treated like others, those power dynamics play a big part. So understanding that and that felt and lived experience for the patient and the provider, and the provider who's also having a very human experience and potentially carrying their own trauma. And even just their own day to day lives. So I always refer to trauma informed care as this practice of being skillful humans together. So thinking about how we use language is significant.
So really, we're cultivating a type of culture in professions who aren't necessarily trained to understand trauma, or to understand the lived experience of those that are oppressed. So we need to do that in ways that are relatable.
So really a real time example of something that we're navigating in this moment is how we're responding to patients that we would consider or might be called disruptive or having outbursts. So even just that language like this is an outburst? And how do we manage de-escalation can feel oppressive to that person and feel marginalizing or dismissive. So what if we change that language a little bit? But then how do you how do you train the provider to think about that?
So on another hand, if a patient came in with a limb, that might be symptomology of an injury in the leg? So looking at an analogy here, if a patient comes in with behavior that feels outside of cultural norms, so an outburst for example, that's a symptom, perhaps of trauma, or that something has happened to this person, not that something is wrong with this person.
The neurobiology of trauma, so what does that really look like? And how does that show up and, at the same time, needing to equipped ourselves then with those soft skills of compassion, active listening, of self care, and all of this needs awareness.
So for example, a provider, taking that pause to ask themselves, how am I doing in this moment? How am I really feeling in my mind and my body and my heart? And in the midst of the culture of health care, how can we possibly take care of our nervous system? It's fast, there are expectations around time. There's a lot of complexity. You're up against a lot, especially now when one of the things that we're up against his staff turnover and being short staffed as a result of the pandemic.
So all that being said, at our health center, staff wellness is emphasized on a regular basis. It can't be just something we say on paper needs to be ongoing. And one of the skills that we use is the practice of mindfulness. And mindfulness supports these qualities of compassion, active listening, self-awareness and self-regulation. You can't regulate yourself, if you haven't checked in to begin with to know that you need it. So becoming more self-aware in our relationships with one another, again, this idea of being skillful together. Some of the ways they we do this more practically, is we at the beginning of our meetings, including our huddles, we have check ins “How are you feeling in this moment? Do you need any support today? And who can you ask for that support?” And these are some of the questions that come out of the sanctuary trauma informed care model. So I want to make sure to give them credit.
We have moments of mindfulness at the beginning of most of our meetings. It could be real practical mindfulness, maybe we're doing some breath awareness, maybe some body sensations and grounding. We have created physical spaces for respite rooms, so that if staff need to step away, because often in healthcare setting, you don't have privacy during the context of your workday.
We have daily practices at lunchtime, whether it's a yoga practice, meditation practice, maybe engaging in some art or music therapy. We are fortunate to have a fitness center on site. And I realize that not everybody has these things. But there are ways that you can create these things. All you need is a room. You could put on a YouTube video, and you could do yoga together for five minutes, or you could do a five-minute meditation. So there are always ways to make these things work.
And another thing we find very helpful is visual cues around the building. We have gold stars all around the building. And they're reminders for you to pause and to check in with yourselves. We asked staff to submit quotes of affirmation or encouragement. And then we have handwritten signs all around the building that staff were asked to hang in places that felt relevant to them are felt visible to them. So as they move through the space, and as the patients move through the space, they see these.
And last example offer is we created something we call the mind body toolkit. So it's both a visual cue that hangs, it looks a little different right now because of pandemic. It's more technologically oriented, but their visual cues and primary care tools that both the patients and the providers can use to help themselves to pause. Maybe it's little signs of affirmation, or breathing practices, or even a stone just to hold for sensation and grounding. Another benefit of that in addition to helping someone just kind of get settled, get present. It improves the relationship between the provider and the patient so that they can they can be humans together while still attending to the to the needs of the visit.
JILLIAN: Thank you so much. Yeah, I'm thinking about how you're giving very concrete examples of how both the care team, the members of the care team, and those that are in the health care delivery setting are also working on themselves, and at the same time able to support the patients that are coming in. I'm imagining that creates an environment where patients feel this sense of comfort that they know that there's work being done on both sides here. It's not just as one direction of I'm being told that these are things I need to work on, but that in fact, the entire environment is committed to being trauma informed, and also supporting the health care team. So I'm curious, Sara, from your perspective, and from your lived experience, as well as the expertise you have with training health care providers, what considerations around trauma are you highlighting for providers and the health system to keep in mind as part of their delivery of care?
SARAH: Where I usually try to meet them, the providers is with what they're experiencing. And I do that with whatever community I'm working with. So when I am doing a training, I'll always say, as you know, is as to my community, you'll find that we're not always the easiest patients to have or to deal with. We sometimes have short fuses. Sometimes we seem angrier than other patients. Sometimes, we’ve got a, what they call a hair trigger for switching a friendly hello into something escalated. And I think understanding a little more about what happened to this person on the way to this visit.
I worked customer service for a lot of years in retail, and I learned that no interaction, even with an angry customer, it's never about me. So, with our patients, they have had, ongoing trauma throughout their, say the last month. They may have had 50 things happen to them. Some of the things may have happened on their way into the meeting. Sometimes people feel empowered by picking on people they feel are fair targets that they can get away with. People get misgendered, rejected by their families. Some have lost jobs.
I’m at the intersectionality between undocumented asylum seekers, Latino community, and then we have a lot of substance use. This is just in our general practice. So I think to some of what Kathleen was saying is, you know, we got to have a team attitude towards this, you know. What I love about my clinic Health Care for the Homeless is that it is always a collaborative effort from CEO all the way up to the patient, you know. And we are a team, and are always checking in with each other. And it's a genuine thing, which is, I think, in some ways, you know, rare and wonderful.
But back to the patients, you know, they'll come in and they'll be upset, maybe you use the wrong pronoun or something. And the easiest way to deal with this to say I'm sorry and move on. But in understanding or having some sort of a picture of what they may have going on in their lives.
If you take a step back, take a breath, and realize, you know, it's not about you. And then don't patronize because that's another one of our triggers. We know when we're being patronized, and somebody's being insincere. But I think just, by seeing another human being somebody's kid, somebody, sibling, maybe somebody's spouse, or parent.
You know, that this is a person just like me, that goes a long ways. Kathleen mentioned about patients, feeling like they're listened to. One of the greatest things, twice, I've had it happen in both points in my life, were turning points where I met a new group. Well, the second time I met a group of trans women from Cambridge. They were all Latinas. And I remember going down the list of the mess that I was in at the time. I was going through a divorce, I wasn't going to see a paycheck for the next 15 years because of my own sense of shame. I had taken on all the marital debt. I was still trying to be as involved with my children as I could, working couple jobs, with no money to no place to live. And on and on and on. I remember talking to this just wonderful, beautiful, trans woman from the community. And she listened to me and she says, ‘Oh, that sounds about that sounds about right. That sounds about like most of us what we're going through. I believe you.’ And just those three words, I believe you. It just means so much.
And I found it, you know, going across to other groups that we work with that that really helps a lot. If you have a patient, maybe who's coming from a vastly different culture and or somebody that's dealing with a mental illness, and they're having things that we would consider not necessarily real, but we can still believe that it's real to them, and kind of get in get in to tell me more about that. That sounds really scary. And you can be real about it to do other people see this person talking to you or is you know, just like is it just between you and them. You can contextualize it and kind of get into it and just be supportive of them. And that's a good place to start. Once they feel listened to you can start building up from them.
So back to us being rough patients. I always say you know, you may be the first person in a month to give us a break. So maybe you don't understand this patient in front of you, you don't understand why this is, this is such a challenge or obstacle for them why this is such a struggle. But just that human contact, that genuine sense of I believe you. Let's start here, let's start working on these things right now and see where you are in a few years.
JILLIAN: I hear a lot and what you're both saying the power of listening, and seeing people, being with people. And in so many ways, it's speaking to really supporting that psychological safety that I don't think is often considered and sort of the flow chart, you know, how the patient flows in and out of the clinic, and, you know, all of the logistics and operationalizing that we do to ensure that our medical system is functioning. We want to put the human back into the center. And really considering that psychological safety is as important, I think, in many ways as to, you know, finding the right diagnosis and continuing to build on the right care plan and making sure the medication is correct. And are you seeing psychological safety? Or something along those lines being part of how you consider care that's being received? Or if this is quality care? Is that part of the conversation for either of you?
SARAH: Yes, actually, it's been astonishing. My nurse and I, that I partner with, in a lot of the trainings, we were invited to be part of the transgender Task Force at Boston Medical Center, when they outwardly declared themselves as having a comprehensive trans care component of their practice. Now, that's not something anybody would have advertised 15 years ago. But strangely, Healthcare for the Homeless did 13 years ago, and I keep telling my nurses how unusual and wonderful that is that they actually said, Oh, no, this is what we want. It's it wasn't like the last thing on the list. It says, No, we're a transgender clinic. And everyone's like, wow, that's different. Because there's so much stigma back then.
So a big part of Boston Medical Center, and we see it all around town is just posting like, little diversity stickers, or flags, or a transgender flag. A GLBT flag is one that includes people of color now, it's sort of like a universal flag. And I always thought that, you know, considering the trauma that we go through, like, you know, what good is that gonna do? But amazingly, seeing those around, like, I see them around in town where I live. And it's an amazing psychological relief to realize that not every transaction I might have is a person who's a little different, could escalate into you know, somebody calling the police or something, some awful, you know, new trauma. But seeing that little flag, it's like, okay, this is a friendly place, these people have had some training. My mind hasn't really prepared me from how much of a psychological relief that is. So, I think, you know, like, as far as communicating safety is to meet people where they're at, call them what they'd like to be called.
Obviously, we have to record them certain ways, you know, to have to do with documenting interactions, records, taping and then the important part of billing. But still, most every one in the world has a nickname and some really love their nickname better than their name. So, you know, even with, if you apply that context onto like transgender care, it isn't that hard if you realize that while people have nicknames and you know I'm going to get to know Susan and she wants she/her pronouns. Then there's no obstacle for us to go forward and deal with that, that fever, that rash, that internal pain. And, again, it's the personal connection, I think that does have the healing.
JILLIAN: It really sounds like you're embodying the practice of mindfulness that Kathleen was sharing with us earlier that you know, being with and that presence and that skill of listening and keeping that loving kindness, that openness. It's a beautiful thing. And as you mentioned, it can be very enriching, it fills you as you're working with others. Thank you for giving us that insight. And, Kathleen, I'm not sure if you'd like to share anything on this as well. But this idea of the psychological safety, and that there is an opportunity to build skill. I'm curious if that's something that you all are working on at your health center?
KATHLEEN: First, I want to say appreciate so much of what you're sharing, Sara, and how we can be kind of saying the same things, two sides of the same coin. Right. And, and that skill does take practice. I think we could all relate to that. I also really appreciate the use of the language around psychological safety. Because I'm pretty confident we don't say that explicitly. But that is what we're talking about. We might say creating safe spaces or understanding where someone's coming from. And I once heard someone talking about medical providers, not so much a specialist, but partialists. So not thinking about someone's psychological experience when they're there for a liver condition. But that liver lives within a body that lives with the nervous system that has thoughts and feelings and memories and experiences and whether we want to or not, we always bring all of that to the table.
So this is a piece I'm going to take with me is this use of how do we talk about psychological safety and its relevancy within the context of health care? But yes, just to reiterate, first of all, know what we are bringing to the table, right? This skill that you're talking about Sara, and the ways that we can do that. And maybe that's maybe that's a pause before you walk into the room. Or when a conversation does feel a little challenging, giving yourself that moment just to feel your breath. And maybe prayer is significant to you, make that part of your day, or music or whatever it is. Do the things that remind you that you are present with yourself and each other. So that could look like a lot of different things. You mentioned the flag, Sara, that gave a sense of like safety and welcoming and having the visual cues that let the patient community know like we see you. This is why we're here. We understand. Or we're trying to understand where your lived experience and be in relationship with one another. So I shared about some of those visual cues earlier. But we get feedback all the time, like you're saying that that that does create a sense of comfort. And it also reminds us as providers every day when I go into the building, I see the sign that Black lives matter and it's like yes, I'm going to reaffirm that again because I'm a white woman from the suburbs. Seeing that sign is important to me to remember whose community I'm walking into.
Also, we're very lucky that we're an integrated model of care. So we have behavioral health providers within our primary care setting that can be available for visits. So maybe someone is coming with some additional psychosocial stressors, and they have the option to meet with a behavioral health professional, or an option to be connected to someone like myself that might connect them to wellness services. And again, remembering that could be many things. So maybe it's yoga, maybe it's meditation, maybe it's fitness and exercise. But because these auxiliary services are there, at the very least making that part of the conversation with the patient, like what are the other ways you're taking care of yourself. And also remember, it can exist within a silo, right, that this conversation needs to live outside of the visit.
So Sara mentioned, and reiterated the idea of team support and reflecting with one another and getting feedback from one another and how important that is. And one thing I have observed, especially in the beginning or with new staff, kind of asking the question, Can I really talk about these things? Can I as a white provider, say, or as a heteronormative provider say, this is how I showed up? And I'm not sure I did it so skillfully, right, because there's that fear of losing your job or punitive response. But if we're thinking about the culture, systemically, like in the bigger picture, then we need to be creating resources to support those providers to educate them. So we can lean towards learning and change and growth as opposed to behaving out of fear that maybe we're gonna mess it up. So that we're creating supportive environments, just for the psychological safety of both the staff and the community members.
SARAH: I've had to work across the lines with, you know, in a way with people that it's, it's not typical protocol, to do certain things, say certain things. And we really have to be adaptable. You know, I think of my own case, I was prescribed my first prescription of hormones about 20 years ago, that for a medical provider to prescribe that as an which is actually an off label, application of this medication, I had to sign forms that, you know, I was taking responsibility for the consequences of that. Now, we no longer do that in medical practice. But even then, I respected the fact that they were taking considerable professional risk to, to get me what I needed. So, I know like, for another example of working with patients, like I said, I work have worked good deal with the Latino community. The people that needed our services, the most, were people who were also asylum seekers. And sometimes when they go to the medical provider, they're very afraid to tell much of their situation. They're afraid to tell of maybe some illegal free silicone that's been pumped into their body because they don't want the medical person to look down on them. There are times they generally don't want to give or they’re very afraid to give the personal information even for records keeping. So we have to hold that precious.
And sometimes we may have to lose a recordable just for being able to help a person that's got a very serious condition, and we have to meet them where they're at, and accept that they haven't really given us the correct information. But I think you know, as healers, and if we remember that we are healers, I think, you partnering up with a supervisor actually helps to try and you know, work out something that you might not have felt, whether or not is was this okay to do this. But at the same time, if we remember, that we're healers first and foremost, we're community members, and that this person coming to me, the thing I always put my mind, is just me on a bad day. Or this is me in a parallel universe, that is another life. Personally, I've had the chance to live in two separate universes that are right alongside each other and I can tell anyone who's ever lived as a male or a female that these are not the same universes. There they are exactly alike in the same space but the life is and experiences and pushback we get through life from our surroundings and expectations about us are quite different.
Sometimes I just feel almost like inadequate, because I haven't been through some of the things that these folks have been through. But again, I believe them. And anything I can do to help them remain stable. In this community that I work with, you can go from years of stability into absolute chaos in an afternoon. Just it could be over, you know, any component of the, the balance of what they have put together for life, it could be you know, housing, something goes wrong in housing, maybe a troublemaker neighbor, or a Saturday night transact interaction with a What started as a friendly face turns into a police encounter. And that just is the first domino in what could devolve into extreme chaos.
So when we're working with patients, we'd like to start out long-term relationships and get to the place where we find other ways of coping, other ways of solving problems of helping patients understand that by doing that they there, yes, they have a pile of 50 problems on it. But even in the condition they are with the choices they're making, we can say, okay, you know, I see this mountain of problems, why don't we work on one. Or part of one. If one is too overwhelming, let's work on a part of one today and see how that goes, see if you're in a better place after we do this a few times.
JILLIAN: When I hear this story, I hear so many aspects of empathy, you know, being greatly empathic and being unconditional with your positive regard of a person, regardless where they are. And it feels rooted in building trust, like you just refer to this long-term view of this person's healing, that it's not transactional, it's not happening right now. I really appreciate that perspective, and that you're seeing people. There's so much to take in here. And basically, what we're talking about is how do we all become more skilled humans with each other? In theory, yes, we get that. But in practice, in what ways can we continuously improve our ability to interact with patients through trauma awareness approaches? And, Kathleen, I'm wondering if as we're kind of wrapping up, what has been your experience with that kind of continual improvement of the interactions with patients through trauma aware approaches, and in that, as you put it previously becoming more skilled humans?
KATHLEEN: I think continuous is the key word here. This becomes the norm in our practice. And that's going to take a lot of work. So I think one approach to that is perhaps creating spaces for practice and reflection. And what I hear time and time again, and I'm sure many nurses can relate is, the time for that is challenging, right. But once it becomes part of the culture, it's not something that we make space for. It's just something that we do, right so that we do need champions. So identifying champions within the workplace, to hold ourselves and each other accountable to that has been really helpful. And also questioning our own workplace cultures, let alone our culture broadly.
But just even in the last couple of weeks, I've had several interactions with individuals that we might be collaborating with that said, I'm so sorry about the delay, I've actually been sick. And it's like, oh, my gosh, of course, please do need more time to take care of yourself? And what they say is, Wow, thank you so much for saying that. I wish everybody would say that. It's like, wow, we're really not giving each other grace. And then we could definitely assume that we're not really giving ourselves grace either.
And remembering that our health is just as much about our minds and our emotions as it is our bodies. So practicing that right for ourselves and it is a muscle that needs to be exercised because culturally we have been exercised the other way around. Like do more, produce more, do more, produce more. And that's really not going to be sustainable for us. And I think we're definitely seeing that, especially with the kind of increase in mental health needs, collectively, is just a sign of something that's always been here, we're just feeling at a different level right now.
And again, just to reiterate that this is a journey, it's not something that we do. And it's done that we need to stay in the conversation, we need to reflect on ourselves, we need to reflect on each other. And just to highlight something Sara, has been saying in so many different ways, and I really want to reinforce it because I completely agree with you, Sara, is learning worldviews. Learning about other people in the way that they see the world and that there isn't one way to be or one way to behave. And knowing that sometimes an expression of anger might be very culturally normal and healthy for that person. Your reactivity to it is your reactivity. So kind of learning about how we can live in contrast and one another and how we can change for perhaps our own perspective, so that we can work in concert with one another. And I think we'd see a lot of growth if we took some time to do that.
SARAH: Kathleen, I think I hear you on the time constraint as being like the number one challenge that we face, because our interactions with the patient can be very short. But you know, I was speaking earlier about being in parallel universes. One thing I've noticed. Now, I would say a large percentage of nurses are female. And there is a superpower that I've never heard somebody a woman speak about. But I've observed that happening all over the place. And that is the ability to be interrupted in the middle of a conversation with someone and then go through any number of transactions, any number of phone calls, additional like parade of customers, paperwork, responsibilities, and then the next second there with the person. In that quiet moment, she's able to pick up the conversation right where she left off. Like, and that is a remarkable tool that I see even nurse providers provide for their patients. Because maybe the next appointment won't be for two weeks or a month, but it's very, you definitely have the skill to pick it up right where you left off and say, Well, last time, you know, we were talking about this. I wish we had more time. But let's pick up right there where we left off. And this is a marvelous skill to give a person as a patient, a sense that they have a connection and ongoing connection. They have somebody that is a champion for them somewhere in their universe. And having just that one other person in life that you believe cares for you can be all the difference in the world about not just surviving, but eventually getting to thriving and being grateful and more content with one's life.
JILLIAN: As we wrap up our conversation, would either of you like to share any final thoughts with our listeners?
SARAH: Just my gratitude towards the nurses that I've had in my life. And I think the people who have honestly helped me the most gave me you know, the time of day, who gave me a perspective that I hadn't even considered. And back to the main point who believed me when I came with this huge bundle of or I should say, like a ball of string that was very tangled. I just would like to just express some gratitude towards any listeners who are in nursing or the surrounding support people, just how important your work is, and how you really do make a difference every day. You have to often do things that are not necessarily in your job description. And certainly, you could get by quite nicely or maybe with less stress by not taking on that little bit extra. But time and time again, I've seen nursing staff do that. And for me in the last 13 years that I've had my primary medical care at Boston Healthcare for the Homeless, I have just felt like you know, it's like an ongoing relationship. It's like family. And for those of us who have perhaps lost that, it is a very important part of my mental health and sense of belonging in the world. And nobody seems to be more willing or able to provide that for fellow human beings than nurses. So my great thanks and deep gratitude to all of our listeners, and to you.
KATHLEEN: You said it so well, Sara. I'm glad that you did. And it brought me back to something you shared earlier is that it is difficult work. And sometimes it feels personal, but it's not about me. And you've mentioned, the mindset of I get to do this work, right. So kind of the same flip side of that same coin is reminding healthcare providers and nurses of the privilege of doing that work and sitting with that in a deep and meaningful way.
Again, give yourself a little grace, definitely taking care of yourself. So we can keep taking care of each other and remembering that seed of what motivated you to do this work to begin with, because I think sometimes we do get a little lost in the woods. And coming back to that gratitude of that we get to do this work, why we get to do this work, and giving ourselves some breathing room so that we can get up and do it again, the next day with that same motivation.
JILLIAN: Thank you, Kathleen and Sara, for joining us on At the Core of Xare and being a part of this conversation.
SARAH: Thank you.
KATHLEEN: Thank you.
CREDITS
Support for this episode comes from the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS). It is part of an award totaling $550,000 with zero percentage financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government.
You can find our most current and past episodes of At the Core of Care, wherever you get your podcasts or at paactioncoalition.org.
And to learn more about the issues we talked about today, check out a related training webinar we have available online. For the link, head to our show notes wherever you listen to your podcasts. You can also access it through the resources at nurseledcare.org.
You can stay up to date with us on social media at @PAAction and @NurseLedCare.
At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder.
I'm Sarah Hexem Hubbard of the Pennsylvania Action Coalition.
Thanks for joining us.
SARAH: This is At the Core of Care, a podcast where people share their stories about nurses and their creative efforts to better meet the health and healthcare needs of patients, families and communities.
I'm Sarah Hexem Hubbard with the Pennsylvania Action Coalition and the Executive Director of the National Nurse-Led Care Consortium.
As part of our special training coverage, we’re bringing you a conversation about the role community health centers can play in addressing community violence. Two community health professionals will share their perspective with us, and how they’re working to improve access to health care and reduce violence in their communities.
My colleague Jillian Bird, director of Training and Technical Assistance at the National Nurse-Led Care Consortium, will lead the conversation. Through a wide variety of ongoing programming, Jillian and her team help support providers working at community health centers across the country.
MUSIC
JILLIAN: Thank you, Sarah.
Joining me for this conversation through Zoom are Cheryl Seay and Wayne Clark. Cheryl is the Program Manager for the Center for Community Health Workers at Penn Medicine at Home. She's based in Philadelphia and is also the founder of the Jarrell Christopher Seay Love and Laughter Foundation, which is focused on addressing gun violence and community health. And Wayne is connecting with us from Oakland, California, where he is a Health Navigator at Roots Community Health Center, Inc. He's also the Founder and Executive Director at Oakland Impact Center, which provides innovative counseling, mentoring, skill building, violence prevention trainings, and more as we'll hear.
Welcome Cheryl and Wayne to At the Core of Care.
CHERYL: Hello, thank you.
WAYNE: Thank you.
JILLIAN: I appreciate you both coming together to talk about this topic. Could you start with telling us about why you do the work you do and what brought you into the field of community health? Cheryl, if you could go first and then Wayne.
CHERYL: I've always been a community servant, so to speak. Just from growing up and observing my parents, they were always givers in the community. And that just carried over into me. And then, you know, after I was married and got my own family, we did the same things. We were the block captains on the block. Everyone came to our house for help and support. Money for heating bills, or the kids would come for popsicles, or we were the family that did everything with everybody on the block. We always supported the children, we always supported the families. After a while, I was working in the university. And my job was discontinued. But then I was offered the opportunity to work as a community health worker on the medical side. A friend of mine said, you know, you and your husband, you're always helping people you do all these great things I think you will work well as a community health worker. So that's how I landed in the role of a community health worker at Penn Medicine. And then recently, I was promoted to Program Manager for about eight months now. So that's how I kind of got into this role and this work, because that was something that I always did naturally.
JILLIAN: Thank you, and Wayne.
WAYNE: Thank you for sharing Cheryl. I could feel the passion from the work you do. I highly appreciate you. Yeah, for me, it was kind of coming through, once being a part of the problem in my community that brought me to the work. I came up in a home where I was a single mother, three boys. I was the youngest, all different fathers. My mother moved to California from the East Coast by way of Little Rock, Arkansas. And we struggled really, really bad. As the young one, when my brother went off to college, my mother was sick. My middle brother was kind of the black sheep. I made some decisions to try to help my mother and help my situation. You know, we didn't have PG&E a lot and food a lot. We were the families that Cheryl was talking about helping.
And so, for a long time, I lived the life being part of the problem in my community. But around the age of 33, I'll be 46 in a month, lost a few really, really close friends to gun violence. Lost one of my friends to life in prison, and this was my closest circle. And kind of a light went on. I have children four children and I always committed myself to since I didn't have my father, I wanted to be the best father I could be. And the light kind of went on and said, Man, this going to be the end for you, prison or death if you don't change something, and we committed to being good to our children.
And in that journey of transformation, I started just realizing that I had never really heard this conversation around healing and trauma. And so it hit me like a ton of bricks like, wait, I'm not just a product of the thing. I'm not just this animal that people paint you out to be, but there's trauma in our communities.
And so as one who always has been what I call investigative, I started to really do a lot of research on this stuff and say, wow, I found that the core of the troubles in our community is the trauma. And then I started understanding that this is historical, you know, from my ancestors. And so taking this deep dive of understanding that our community is traumatized over and over and over, it made me start to take my own journey. And as I started to heal and be proud of myself and progress and do amazing things, I just wanted to offer that to everybody else in my community, because I know now that the possibilities are unlimited. And I actually also say that we the people who have been through the problems is the people who can help the people that are going through the problems. And so there was nobody more qualified. And so finding myself in these spaces, I came to Roots in very intentional because Dr. Noha, who was the Founder, Executive Director, was one of the most powerful voices I heard that was connecting health to violence.
And I really hadn't started to hear that until about three years ago. And that caught my attention. Because I'm like, yeah, the root of the violence is health issues, mental health is all kinds of health. And then at the root of a lot of the health is gun violence, too, because you get the mothers and that are going through all kinds of stress and the families, it takes a toll. And so I came to Roots, because I wanted to be close to the voice that I knew that was doing major work. And healing has been at the core of my journey. And so that's kind of what brought me to the work is that I was once a part of the problem. And I passionately now like to serve and be a light, and make the connection to y'all. We not just like this, because we are but we need healing. And we're a traumatized community.
JILLIAN: Thank you both for sharing these reflections on your community and your lived stories. I do really hear from both of you this desire to be available to your communities, to give back to your communities. And it's given you this opportunity to interact directly with community members in an effort to improve lives on a personal and broader level. I’m wondering Cheryl, if you could give us an idea of how your life story or events of your family have directly given you cause to address community violence within your community here in Philadelphia?
CHERYL: In 2011 you know, my family's life changed forever. As I mentioned before, we were always the family on the block where everyone came to. But on April 24, 2011, Easter Sunday, our family had just finished Easter dinner. And these two guys rang the doorbell. And my husband said that he got a funny sense when he saw these guys at the door. They were asking for my son Jarell, who was in the basement preparing for school, it was Easter break. So he was getting ready for school the next day, washing clothes and doing all those type of things. And so my husband called Jarell to the door, because Jarell knew everybody. He played basketball, like everybody knew him, all the children loved him. And he went outside on the porch. And my husband said he went with him because he just didn't feel right about these guys. And so they asked Jarell a question. And Jarell said, I don't know what you're talking about. Now, Jarell is six feet tall, six two, 200 pounds. And so he talks to the guys, tells them that he doesn't know what they're talking about. He turns around to go back into the house, the guys make pretend they're walking down the steps. And as Jarell is going into the house, they turn around, and one of the guys shoots Jarell in the back twice. And he falls at the door. And my husband is screaming, and I'm screaming, and the neighbors are screaming. Everybody was outside. And I couldn't open the door. It was just the most horrific day ever. Like, it'll never ever, ever, ever be the same for me or my family.
And we felt like we were betrayed, because we had been a family that was always giving on the block and helping others. And now this happened to us. And nobody was saying anything. Nobody said they saw anything. And it was a beautiful day outside, it turned the darkest day ever. Even now 11 years later, you'd look around and you see these things have gotten even worse. These shootings are happening every day at anytime, anyplace. And it doesn't seem like anything is getting better. And so we started the Jarell Christopher Seay Love and Laughter Foundation because Jarell always gave us love and laughter. Every night he would tell us love you Mom, love you Dad. You can imagine this six foot tall guy. [Laughs] You know, sharing that love. And that's who he was. As I said, all of the children in the neighborhood loved him. Even the little children would come to the door. Is Jarell home? Can he come out and play basketball? Because he was just that type of guy. He always looked out for others, the elderly, the children. He was always there to support others and my other son as well.
And so we developed the foundation. And the mission of the foundation is to unite communities by connecting families while helping to protect our children through gun violence prevention, safety, and education. And through our organization, over the past 11 years, we have worked with the youth in our community through different programs that we have offered.
One is the defenders program. Then we have another one, the LIP program, which is Ladies In Power for peace where we mentor young girls. And through both of those programs, we empower our youth to know that they don't have to let their current life circumstances determine their destiny. We also teach them about their history because they're not being taught their history in school. We also teach them about being a good citizen, knowing and understanding the process of voting, making sure that they go for their driver's license and their voter’s registration and the things and life that they need to be successful. And we also empower them to be involved in their community and perform community service activities.
JILLIAN: I'm sitting here listening to your story, start from such a profoundly, intensely tragic event. And what I'm hearing you say, the end here is how much you've kind of doubled down on loving your community. And when I imagine, it could be very easy to want to retreat into anger and despair. And it's a really profound story and the way that you've put into action, emotion and loss. I wonder about that resilience, and you speak about healing, including the whole family. And I know that this touches on a lot of the work that you're doing Wayne and just interested to hear how Cheryl's story is resonating with you and where you see your work intersecting with Cheryl's and how your efforts are directed at healing?
WAYNE: Cheryl, thank you. My heart is full, and also heavy at the same time, but just a lot of celebration. Man, we are such resilient and powerful people. And that's the message I want my life to carry is that you can take your pain and turn it into power, you know, and you can take it and we have choice. Our work, it's so much, you know, at the heart of it, it's so similar because my thing I started my particular organization, after working with a lot of different organizations as a contractor and working mainly like with the city of Oakland, and then I did some work with the city of Flint, too, as a consultant. And one of the things that Cheryl pointed out is that it's not just about the children, it's about the whole family.
And so even in a lot of my work and starting my own organization, one of the things I had was a container called Brothers Behind Mothers. And the reason why is because as we were working with a lot of these, you know, young men caught up in the cycles of violence, a lot of my work was working with the perpetrators and the victims. And so what I started to realize is, this saying came out of it, that we're working with the fruit. But what about the root? Which is the mother's a lot of times, you know, we have so much work, I just have a belief that you know, and even out of my own story, like if, if you would have came in and really took some time to see why like why I was being who I was being at the age of 15, 16, 17 and these early ages, you would have saw my mother was in the hospital for eight months, one year. We were struggling with no finances, P&E was being cut off. And my mom was doing the best she possibly could. She was doing the best she possibly could. She is my She-ro, and she was doing the best with the cards she was dealt but it just wasn't enough. There wasn't resources. Nobody was really coming to help. And so one of my passions have come out of this understanding that, okay, I can sit with a young man. And I've had many of them tell me this over and over, they say, Mr. Clark, I sit with you for an hour or two, and I feel like I can do anything.
Then I go back to the block, and gun violence happens. Now I'm back in fight mode or I go back home, and my mother needs medicine for my little brother. What do I do now? I still know everything you sat and told me. But there's these things going on in my home.
And so one of the things that I looked at when I started my organization, as I said, to work with anybody, I have to do at least one in-home visit to work with us to qualify, because what I've come to understand is when you go to the homes, or go to the community, you'll get the answers on why people were struggling more than anything they'll probably tell you when they can sit down and because they can't really articulate everything that's going on in their lives.
And so in this process of seeing all this, knowing my own story, knowing of all my friends story, it really has become about the family. Because to have this healing work be sustainable, you can't heal one person, and then they go back to the pack. And it's still trauma. So I have a passion about working with the mothers. I've really done a lot of research on what I feel like we're being reactive, so you can look it up, and we have much money on reentry. But then there's not the pro-active work, you know, like Cheryl is talking about working with young people. I mean, I've built this passion where I want to start working with the six- and seven-year-olds, because the times is changing. And these young people are carrying guns and they know all about everything. And they're carrying the trauma and we understand that this path of trauma.
And so when Cheryl talks about the family like that lights my heart because that is what I think I don't see enough, I see a lot of organizations working with the individual. But actually, we need this holistic healing.
I have many young men or young women that you know, we work with them, and then they go back home and the family don't understand what they're trying to do anymore. So there's a lot of alignment, I believe that the healing it really does have to happen holistically. But I think we definitely need to be more pro-active in our work. And I really would like to see more funds and more intention put into that because, and just even talking about healing in our community, it's taboo.
Therapy, when I first got therapy when somebody came to me five years ago and was like, you know, hey, a good mentor, he's like, I'm gonna pay for your six therapy sessions, because the work you do is amazing. But eventually, you need some help, too. And I was like, no way. We don't do therapy. That's for crazy people. That's what I've been taught. And he broke it down to me in a way it was like, and I was like, I'll try it. So I went and it was the most amazing experience in my life. And so then I just been doing therapy at everybody like Oprah, like you get therapy, everybody needs therapy. But sometime I am their therapy, just my showing up in my in my way with my energy and working on myself. And I think we need to concentrate on the mental, the physical, the spiritual, the whole person, you know, and I think there's a disconnect. So mostly everything Cheryl said is I piggyback and it's the same work I'm trying to do.
JILLIAN: Thanks so much for all of that this comprehensive expertise that you both are sharing with us. And I keep hearing your personal stories and how this is giving you what I consider a special expertise. And you also both work in systems of healthcare, and what an amazing insight you have as providers to navigate through communities and understand the populations that you're working with. Both of you work with organizations that are quite different. Cheryl, yours is a massive academic hospital system that is invested in its community and particularly in the community health worker program. And Wayne, you're working with Roots, this community health center that's really mission-driven, rooted in a community and doing work really focused on the needs of that community. So I'm really curious about the day-to-day ways in which you see the systems participating in the healing and addressing, supporting individuals facing violence. Or on the other hand, and where we are still falling short with our systems? And you both have mentioned a little bit of that up to now, but I'm wondering if you could look at it more from that perspective of the system? And maybe Wayne, you could start.
WAYNE: So coming to Roots was like, it was a no brainer for me. I literally sought them out. Dr. Noha Aboelata from Oakland, California, with this vision that connects health or healing, and violence like you know, and, and built this amazing organization, Roots, that offers the person anything they need pretty much from helping people with medicines to therapy. I'm talking to on like on the spot, you can come to this one stop spot where you can almost get help with anything. I mean, if you need a mentor, if you need to talk to somebody, if you need help getting an ID. She looks at all of this as a part of health. And so that was so interesting to me, because I've never seen anything like it. And so in my day-to-day work, I'm actually a life coach. So that's kind of what I do. But the title was in within Roots is Health Navigator and what I like about that, and it was first time I heard it is because Doctor Noha understands that we're helping people navigate their healing. And so that's why it's called a Health Navigator. Because healing, you know, it's step by step, sometimes just getting the ID when nobody in your family, you know, just having somebody around with good energy and good vibes and positive outlook on life. Or it's just having a good example around.
And this is the work that we get to do. So I'm encouraged by some of what I consider some of the individual systems, which I feel like is a small part. But the bigger systems, I think we aren't there yet. I think we're still struggling as a bigger system to get this understanding that health and violence is connected, that people are not just violent, innately. You know, nobody comes out of the womb wanting to do these things, but there's things that happen along the way.
A vision for me really would be where bigger healthcare places will have more people like me and Cheryl sit at the table in some of their bigger meetings, influencing and giving them not just the book stuff. See, you get all the stats. That don't tell you half of the stuff me and Cheryl can tell you what's really going on. So my vision is, what would it look like if Wayne or Cheryl was sitting with a big hospital and had a voice at the table saying, Okay, I know that's what your numbers show. But let me give you some insight on what's really going on there.
And then on the same side, when I'm out here with all of the workers that's doing the street work, what would it look like for somebody from the health care system to come in and actually sit at our tables. So this cross working.
I just believe this separation, where we don't understand that it's all together. There is no separation really. Many of the mothers that show up at hospitals, they don't even know how to identify that their depression, their stress, or whatever it is, is because I lost a son two years ago, they won't even tell you many times because they think it’s normal. So I really would like to see us crossbridge this stuff. And I am so excited to be a part of an organization that's doing it. But I feel like at this point, collectively we're not doing a good job at that. And so I would love to see more of that in the bigger systems.
JILLIAN: Cheryl, is this leading you to have a response to Wayne?
CHERYL: Yeah, I totally agree with you Wayne on having bigger systems involved, especially our health systems involved in in part of the solution, working towards the gun violence. And it's so ironic that you should mention like sitting at the table with some of these big health systems, because for the past year, me and five of my colleagues have been sitting with the Penn Medicine executives, in a mentorship program, where we've been telling them and talking with them about how we would like to see people of color at the table making a decisions about the care of the community that they serve. Because when you don't have that, then you don't have fair and equal treatment and care. You have bias, which I've seen, you have folks that are just out of touch. They're not into reality, like it's so many things. So if we don't have equal representation at the table for decision making. How can we ever move towards changes? Like we're always on a spinning wheel trying to catch up. So that's a program we've been working with over the past year. It's coming to an end soon. And we hope to have some continuation in thatprogram. But I pray that some positive results come from that.
But also getting back to the other things that you mentioned. I also see, you know, as being a community health worker first before going into the manager role. A lot of the folks that we would talk to and meet, visit and help support often dealt with trauma in some type of way. I've had folks tell me that every man in their life touched them. Some of the older ladies, I've had people tell me how they don't have anything to eat at the house. Or you go to the house. And you see the living conditions where they have holes in the ceilings and the walls and you're wondering, why aren't they coming to the doctor where they're trying to get the house together, because it's in bad shape. And they don't want to come outside because you're free to travel because of all of the things that's going on in the streets. So as so many layers, as involved, that relate to gun violence there have to be addressed. And we do we have to get everyone involved in order to work towards some solutions.
But I've even seen because I've participated in a lot of conversations and some other podcasts and some gun violence symposiums. And I'm glad to see now that is becoming more of a conversation and more people are talking about it. But to also see that a lot of the clinicians or providers that are working in the trauma units are also traumatized. They are also traumatized just because they are already in these professions. And you know, they have a nice paycheck, they live in nice places. That doesn't mean that they're not feeling and absorbing all of this happening day after day after day.
Just like Wayne said, we are all affected by this. This is our pandemic. This gun violence is absolutely ridiculous. And I hope, pray that we all come together every entity, every organization, every party that can be a part of solution come together. Because one thing that's not going to happen and I think folks are waiting to happen is that somebody's going to come in and save us. No one's coming in to save us. This has been going on way too long. We have to do this collectively as one. Then we start to see to change.
JILLIAN: And as individuals as people and health care feels like a system. And what it is when you get basic with it is people supporting other people. And I hear so much you're acknowledging the pain and suffering that is existing in health care professionals lives as well. And there's so much that we do to try to shut those feelings down. Obviously, living within communities that are experiencing elevated violence or so many adaptations people have to make just to get through. And we see it in healthcare systems where people become shut down, they lose that human connection. You know, we've talked about the systems and the impact that violence has on health. Cheryl, you mentioned something almost the effect of universal trauma, you know that who hasn't experienced trauma at this point? I'm wondering if either of you can reflect on strategies that you've seen in practice or you yourself practice that help mitigate some of that trauma that is being experienced in communities, or how healthcare professionals might implement these strategies, in the ways in which they're relating to people that come in for care
CHERYL: Well, I think for the health care professionals, for them to be more relatable to the communities that they serve, that they should have cultural competency training, I know that it's usually something that's required, and they may do like a one-time training or something like that. But I think that's something that should be gone ongoing, because you have to understand the populations that you that you serve, like the things that are their customs, so to speak, you have to know the type of things that they go through and deal with in order to be able to treat them and care for them effectively. You just can't treat them or work with them on what you may think that they should receive or what they should react to. If you don't understand where they come from, like you're not that lived experience like me and Wayne are. So you just can't say ‘Oh, well, you know, They're just complaining because they don't want to lose weight and they just keep eating all the junk food.’
But if you're in that environment in that community where they live at, and you see the food choices that they have, and you see the barriers and challenges, then you're not likely to say, ‘Oh, well, they don't care, or they can't do better.’ You, you say, ’How can we make it better?’
I think that's something that would be helpful, especially with the health care providers and providing like quality care, understand the clients that you serve, and where they come from, would be helpful. And then also too, partnering with like, community groups like the Jarell Christopher Seay Love and Laughter Foundation and Roots. These organizations and law enforcement and senior centers and daycares, and schools, work together collectively, on how we can address these issues. Because like Wayne said, working with six- and seven-year-olds, because things are different, they are very different right now. They are very different in our schools and in daycares. Things that would have never happened 5,10 years ago are now happening, where these kids are bringing drugs to school, weapons to school, babies. And we're not talking about teenagers, we’re talking about babies. So we have to start there as well and include them in. And that's something that the Seay Foundation has done in the past, we went into daycares and talked to children about the dangers of firearms. We have to stop, you know, putting folks in silos or oh, well, these are babies, they don't necessarily need to know about this, because they can't understand that. That's not true. We have to include everybody in this to make it better. So your partnerships is very important, as well as the training for health professionals.
JILLIAN: And what do you think Wayne?
WAYNE: Yes, I 1,000% agree with Cheryl. And just to add to that, I think there's an opportunity. Cheryl brought up one of the greatest points for me, and I think you've heard me kind of already talk about this. As I've looked at people who have done this work, and I'm gonna just call them healers, right? Whether it's people in health care, or people working in the street, helping people heal, we're helpers with people's healing, many times the healer is not getting healed. And so when Cheryl talks about that healthcare person that is struggling with their own stuff, we see it over and over and over. And this is something that scares me really.
I actually have come to my own belief of working around many people who I call my friends, that we have people that run into this work running away from their own work. So it kind of sometimes lets you not focus on your own stuff. But you can feel good about helping by everybody else. That's not sustainable. So I believe, we need more education and more programs for the healers, for those who are actually doing the work. And this is something I am so proud that I've got to be a part of as I've taken this journey. In healing, I'm just understanding that one of the things I tell a lot of people that surprises people with that healing is you know, trauma isn't in your mind. It's in your body.
This simple saying catches so many people off guard. Trauma lives in your body, it is a lived thing. You can say something I can remember my friend being shot 12 years ago, I can feel it right now. Cheryl will testify to this, you can feel it. So it's in our body. So one of the things that has been powerful for me is one of my good friends. We talked about this about five years ago, he’d been working on it. This year, he got a grant, where we brought 10 brothers together from across California, most of them have been incarcerated from L.A. from Oakland to Stockton, been part of gangs, been part of the problem. Let's just say that. But we've all transitioned our life. And we're now doing the work to help our communities. But many of these brothers don't have space to help themselves. So what we did was created create this space called the maroon space. And it's all black men, men of color. Black men in this particular space, and we have had four retreats in Santa Cruz. On weekends. We go up on Friday evenings, and we come back Sunday evenings and it's all doing what's called somatic work. Somatic work is a work that I literally look at it as our ancestors’ kind of work. It's a work where our ancestors didn't have doctors, how did they heal? Well, they knew a wisdom that was in their body, you know, and so many times, our brothers and our sisters, and our healers, and our people are, you know, working with intellect, but there's a higher intelligence that is existing in us that's accessible, that can help you work with stuff. And it's a trip to see some of these brothers who, when you ask them, Where do you feel that in your body, what is your body telling you? They want to go to their heads, but we invite them into, and I'm doing this process to, of tapping into the wisdom of your body, listening to what your body is actually telling you. Many times your body will feel something, you just say, Oh, I had a gut feeling that's a real thing. The gut is the second brain that a lot of people don't understand, you know. And so even bringing that kind of stuff up, just sharing this kind of education about working on our own.
Our own stuff, I think, is one of the big things that I want to see where we're concentrating on getting the healers healing. I've had the opportunity to work with law enforcement.
Kicking and pushing when I first started that work, didn't want to do it. And but I'm always listening to what I call the Mother Harriet Tubman voice that if it says go, I go. That’s my favorite hero. And I went, and it was, it was such a blessing to me, because what I realized is, those are some of the most people that need healing in our world, is law enforcement. The stuff they deal with, like and don't get no help. So all across the board, from our nurses from our street workers from our mothers to when Cheryl says everybody has been impacted by this. Even some of the people that don't recognize when they pushing back on this, there's some trauma there too, you know, it's deep. So this conversation on the healer, getting healed and having access to healing is a big conversation for me. And then, like I said, I do want to continue to think about how we, we really come together collectively, in with saying,
Cheryl talked about our partnering, but don't just partner, but give them partners the same power at some of these meetings, because I see people bring people in to look like a good look. Like okay, Wayne is at the table, but we're not going to listen to anything he really says. But we just want him at the table to be able to say he's at the table. But no, bring people in and value their voices and their wisdom. No, it might not be from a college.
But man, I'm telling you, I have never been to college in my life, y'all, but I've been all over this world. Why? Because once I understood that my experience is something that many organizations don't have access to. You can't get this information. Many people are in those books, and they can read it back and forth, but don't really know how to deal with people. You know the program, I always say, y'all know the programs but don't know people. And that's a problem. You know, so I would really love to see more of our voices valued at the table, you know, actually see follow-through on some of our stuff, but that one with the healer being healed.
Let me say this piece, here's one of the biggest issues, to me, is when we do the work, say myself, let me use myself. And I'm working with these 10 young men, and we're making progress. And then I relapse and leave all 10 of those people what they had hoped for a year. And now I'm going guess what, I re-traumatize them, because they had hope. And I was loving them. And then I did the same thing that every system, everything that has failed them, I did it all over to them again. That's what happened. When you don't take care of yourself as a healer, you can leave these people that you were actually leading and I see this happening all the time. And then people wonder what happened. So sometimes you only get one shot with people. They only trust one person. And if we fail them, then sometimes they'll never give anybody else chance. So that's why I believe it's huge for the healer to actually get help, too.
JILLIAN: Yeah, and just hearing what had to have been an amazing experience for you and the men you've been working with, really makes me think of just how much trust they have in you to put themselves in such a vulnerable position and to trust you enough to open and get into their body and what they're feeling. I think about that kind of experience and what it would be for a health professional to be vulnerable and to be a person themselves in a patient encounter and kind of where that falls away, that ability to be a person relating to another person to provide a space to build trust. I think in so many ways our health care system asks us to completely shut down as people and just address everything like a case or a condition or a complaint. And that heal the healer, I think is a really powerful way to consider it, and hopefully, something that we can see more of in not only our bigger systems like Penn, but in our community health centers as well. I think there must be a tremendous felt burden across all of our systems coming out of COVID feeling the tremendous amount of despair of loss, we've lost over a million people. And we also have a heightening of community violence. And I wonder when you think about your place of work, how are you supporting each other? In your day to day work? Are these conversations happening with your colleagues? And if so, what are you doing for each other?
CHERYL: For us, we take time and set aside and have fun time, like fun Fridays. Just for instance, everybody got a paint kit and a blank canvas and a little easel and we'd had a couple of hours, towards the end of the workday on a Friday, and we all painted a picture, which was a lot of fun. And you have to have that break, as a helper working in that role. Because you can burn out most definitely, you can definitely burn out after visiting and seeing and feeling the things that your patients go through that you have to deal with on a daily basis. So you need that little breakaway time. We've also done activities where we've done ax throwing, we will go and throw an ax, get that frustration out. We've done outings to amusement park. So at our center, we do take time, we'll set aside dates or whatever, to do fun things just to kind of relax and just talk with one another, sometimes bring our families in, depending on the event, and just to get that break in and just to enjoy one another, for who we are outside of talking about the patients or, you know, dealing with the doctors or the nursing staff or whatever. Just to be ourselves. And that's helpful. You know, for us, that's what we do.
WAYNE: Yeah, I love that fun. That's the key. I don't think we even use that word in a lot of our work is you don't hear fun. No, don't you dare. But I think at Roots, there's a culture, that's very intentional. You know, honestly, it's still hard in our communities to try to sustain it. But I think that no highest set a culture where first and foremost, I think we do a lot of education in our in our monthly trainings. And throughout the week she has implemented where we do trainings that are for the staff, you know, here's how this can be showing up in your work. Pay attention to this for yourself, not for the client, and you know, and so I love that about the trainings. She's made the therapist that we have at Roots accessible to the staff, which was one of the big ones for me, now that that's a whole thing within itself because I think everybody right now I know in the Black community therapists are thin because people are finally saying with COVID I need some help, and I can't do all of the stuff and so but I think it's amazing that we have access as a staff to therapists and then creating spaces for fun. We do outings.
We have a yearly get together. We have things that we do on a on a regular to try to create spaces. And I think one of the conversations that has come up is you know in my own life is I tell people I take care of Wayne first. I do not know another black man that takes care of himself more than me. And I'm proud to say that, but it hurts my heart to say that I like I looked at my life. And I say, okay, my first dedication is to my children, how can I be the best father to and what it all pointed back to with me taking care of me. And I had never really heard this. And even in my spaces, were especially talking to my elderly brothers. Like it just they bring it up, like, young brother, y'all have access to things and you're blessed to have somebody, we couldn't even, we were surviving, you know, you all have access to things. So I just love talking about some of these things. But I think it really starts with educating people on how important it is to take care of you, you know, and so I think Roots does a great job with that.
But individually, I’m very fit. I tell people all the time, I don't even go to the gym for my body. I go from my mind, and my body just reaps the rewards, you know. But I'm going because I know what I'm carrying. And I know what my purpose is. And so, to be the best me for my kids first, then the son to my mother and then, to help to my community and to help to the world, I need to be good for me. So I take time I treat myself to movies, I treat myself to nature, I treat myself to travel, which is my favorite thing, but I make sure I take care of me. And so I'm trying to be an example of that. And I think is doing good. Because a lot of brothers and a lot of my people in my community are started saying, I didn't even really know that was a way that was, you know, a choice. And that's a word, just the fact that we have choice. Some we don't even I don't think we know we have choice, that this is a way that you can actually live. Like I tell people, I take myself to the movies, they'd be like, what I'd like it's something I really enjoy, I go sit my butt in the back of the movie all by myself and watch. Find whatever that one, it ain't got to be a big thing, find something that really gives you joy, and get you disconnected from everything. And do a little bit of it for yourself, you know. So I think that self-care, is, you know, huge. And so, I think that that is that is where we're headed. And I think we got to do a much better job at it.
JILLIAN: I appreciate you both very much. And given everything we've discussed today, I'm wondering if you have any final thoughts that you'd like to leave with our listeners?
CHERYL: I would encourage everyone to get involved in some type of way in your community, rather, is to volunteer or it's not always about having to give money because folks may not have it, but you can give your time, an hour or two, whatever it is to be a help in what's going on in our world today. No, we can't solve every problem. We can't fix everything. But even just that one little thing is helpful to someone. And it's also helpful to you as well. So I would encourage everyone to get involved in some type of way and whatever it is that they enjoy, or being helpful with to do that. And also to remember the motto of the Jarell Christopher Seay Love and Laughter Foundation and that is let love be the power that rules you. So with that when you have the love in your heart and kindness and you let it take over, then you will have the positive outcomes.
WAYNE: Beautiful. Yeah, I want to sit with that for a minute. Thank you, Cheryl. Yeah, for me, I just like to encourage everybody to understand that. We all have gifts. I don't care what you been through. In the beginning of my journey. My biggest battle was guilt and shame for all the people that are harmed, but I had to do some work through that. And I had to realize that I am not the things I did. I made some decisions. So I'm speaking to one particular group of people, sometimes questioning how do I serve? It was the first time somebody invited me to speak that lit a light in my heart to understand oh, this is my thing. Oh, I have I have something in me. So, but speaking to like the bigger organizations that might listen to this or the people that are like kind of outside looking in and wonder how I can be a part because I'm starting understanding there's a lot of that I had somebody telling me about a month ago, Wayne until I met you, I felt like I was looking up at the freeway and didn't know how to enter into helping
I want to say this, be really intentional. You're intentional about a lot of things in your life. If you really want to help, be intentional by researching and find a way, there's a Cheryl, there's a Wayne, there's a Roots. There's an organization where you can talk with somebody, I don't care if you come from the wealthiest community. And you've never been to one of these kinds of communities. But be more intentional about trying to help because there are many people sitting on the sidelines, who really want to help and just feel like they don't know where to enter. And I would just encourage to be more intentional, there is so much that you can be. And like Cheryl said, the love is needed. Our world needs love and light, and that's what I'm committed to being a part of the love and light.
JILLIAN: I'd like to sit with Cheryl's motto myself. Let the love be the power that leads you. Thank you both so much. Thank you for digging into this very challenging topic, sharing all of your gifts, all of the vision and hope that you see. And also the reality of how you know how these day-to-day struggles affect people. So, I appreciate you both very much. Thank you.
CHERYL: Thank you for having us.
WAYNE: Yes, definitely.
MUSIC
CREDITS
Support for this episode comes from the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS). It is part of an award totaling $550,000 with zero percentage financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government.
You can find our most current and past episodes of At the Core of Care wherever you get your podcasts or at paactioncoalition.org.
And to learn more about the issues we talked about today, check out a related training webinar we have available online. For the link, head to our show notes wherever you listen to your podcasts. Or you can check out our resources tab at nurseledcare.org.
You can stay up to date with us on social media at @PAAction and @NurseLedCare.
At the Core of Care is produced by Stephanie Marudas of Kouvenda Media and mixed by Brad Linder.
I'm Sarah Hexem Hubbard of the Pennsylvania Action Coalition.
Thanks for joining us.
The Pennsylvania Action Coalition (PA-AC), a program of the National Nurse-Led Care Consortium (NNCC), is thrilled to announce their new collaboration with the Geisinger School of Nursing to address nursing faculty and instructor shortages by creating Nurse Education, Practice, Quality, and Retention Clinical Faculty and Preceptor Academies (NEPQR-CFPAs). The collaborative will execute the program with funds awarded by the U.S Health Resources and Services Administration (HRSA), CDFA#93.359.
The purpose of the NEPQR-CFPA is to take steps to fill the faculty/instructor gap in schools of nursing and increase nursing workforce retention by leveraging staff nurses to participate as skilled preceptors and clinical instructors. The PA-AC and Geisinger, alongside numerous academic and health system partners, will build academic-clinical-community partnerships that develop and implement comprehensive and self-guided nurse education training curricula. The project will focus on HHS Region 3 (including Delaware, Maryland, Pennsylvania, Virginia, West Virginia, and Washington, D.C) to build a formal nurse education training curriculum to train clinical faculty and preceptors.
To develop this curriculum, the PA-AC will assemble an Advisory Board that is reflective of diverse practice areas, academic pathways, geographic location, and populations served. The advisory board will oversee curriculum development and determine metrics for review. The PA-AC will work with Advisory Board stakeholders to ensure that the course content is engaging, thoughtfully articulated, and caters to a wide audience. In Year Two of the project, Geisinger employees across the health system will pilot and evaluate the curriculum. The Advisory Board will use lessons learned to prepare the program for implementation across HHS Region 3 in Year Three.
The PA-AC will work with the Advisory Board and its extensive network to foster dialogue around the program’s goals and outcomes, promote the implementation of the program, and showcase the project as a model to bolster the nursing workforce. Ultimately, the purpose of the collaboration is to work across the region to improve the training, preparation, and availability of clinical nursing faculty and preceptors to better support nurses in advancing healthcare.

The Pennsylvania Action Coalition recently published, “Diversity Impacts of COVID-19” in the journal Nursing Clinics of North America about the impact of the COVID-19 pandemic and demand for social change.
This article describes how COVID-19 health disparities relate to the social determinants of health. In order to advance health equity, the article underscores the importance of a diverse nursing workforce prepared to advance an antiracist framework and social justice. The article reviews recommendations from the National Academy of Medicine’s Future of Nursing reports and highlights practical strategies to promote diversity and social justice, including mentoring nurses from underrepresented backgrounds, amplifying diverse nursing voices, and leveraging the power of coalitions. In highlighting the interwoven impacts of COVID-19 and demand for social change throughout 2020-2022, the article strives to move beyond the acute COVID-19 crisis to sustained social justice in healthcare.
Read the article here